On a January evening in 1992, I was sitting in our kitchen, reading a comic book. My older sister Claudia went out to run an errand at a nearby minimart, just before it closed. Her keys jingled as she said goodbye and pulled the door shut. Her footsteps rushed down the stairs. A minute later, I heard her slam the garage door after she had pulled out her bicycle. Moments later, I heard a loud thud from down the street. I also thought I heard a muffled scream. I was 10. I couldn’t connect the dots.
A speeding car had hit Claudia while she was crossing the street. She didn’t die on the spot. Her boyfriend rushed my mom to the hospital. They spent the night at the ICU, while I spent the night in my best friend’s apartment. We set up camp on mattresses on his living room floor. He said: ‘I’m sure it’s just a broken leg.’ I said: ‘You’re right, she’ll be fine.’ We prayed. The next day, my mom stood in the doorframe, sobbing. ‘Claudia is dead,’ she said. I hugged her. I knew I had to be strong for her. What I did not know is that my sister’s death would, in some way, end my mom’s life as well.
We cried at the funeral. We cried at the cemetery. We cried at home. After a few months, I stopped crying. My mom never stopped crying. She became obsessed with Claudia’s grave. She would visit it every day, clean the white marble and bring fresh flowers. At the same time, she became frustrated and angry with the world. I spent my entire youth listening to her angry words, but her grief wouldn’t recede the tiniest bit.
Somewhere in my teens, I concluded that she must be suffering from depression. But I was wrong.
It’s no surprise I had it wrong. Back in the day, even professional psychologists lacked an official diagnosis for persisting grief. That changed in March 2022, when the condition my mom most likely suffered from was added as ‘prolonged grief disorder’ to the latest revision of the psychologists’ diagnostic manual, the DSM-5-TR. The diagnosis hinges on two factors. The first is denial: mourners cannot accept the death of the person they lost. This, in turn, causes symptoms like sadness, anger or guilt that last for more than 12 months.
That persistence separates normal from prolonged grief. While the former is like a wave that occasionally flares up and then ebbs away, the latter runs like a horizontal line. Prolonged grief traps its sufferers in continuous rumination. This causes the second diagnostic factor: impairment. Some sufferers quit their jobs; others avoid people and places that remind them of their loss. Avoidance is just one of many hallmarks of this disorder. While guilt, self-blame and anger rank high, one of the most prominent symptoms of pathological grief is the loss of meaning in life. People who get stuck in prolonged grief often see no point in living without the person they lost.
This matches what my mom said. Twenty years after Claudia’s death, she would still say: ‘When your sister died, a piece of me died with her. I will never be alright again.’ She would stay alive as long as she had to. The only thing she looked forward to was being reunited with Claudia. If she got cancer, she’d refuse treatment. I offered to help her find a therapist, but she scoffed.
It is how people die that determines whether the survivors will develop the disorder
Caring for me became her duty, but not a pleasure. I didn’t understand why. But now, a study by researchers in Japan and Italy shows how prolonged grief lowers empathy. The scientists showed bereaved people photos of their deceased loved one and other photos of a living relative or stranger. They then measured those individuals’ empathic response in an fMRI scanner. The result: the more patients were grieving, the less empathic they were with living relatives. Their empathy to the dead person was enhanced.
My mom wasn’t an isolated case. Between 7 and 10 per cent of all bereaved people develop pathological grief, a large study from 2021 shows. When the number of deaths went up during COVID-19, the number of pathological grievers, naturally, went up, too. The uptick was not just caused by the numerical increase of pandemic-related deaths. Rather, it is how people die that determines whether the survivors will develop the disorder. ‘If you unexpectedly lose a close person, you are much more likely to develop prolonged grief,’ says the clinical psychiatrist Katherine Shear who heads the Center for Prolonged Grief at Columbia University in New York.
Sudden loss includes death by murder, suicide, accident or an unexpected illness, like COVID-19. A loss may become more traumatic when you don’t have a chance to say goodbye. What ensues is often a feeling of powerlessness. Personal factors, like female gender, low education and an existing mental illness, further increase the risk of developing prolonged grief later on, as the psychiatrist Andreas Maercker writes in his clinical handbook Trauma Sequelae (2022). Being part of a tight-knit family and curating a circle of close friends, on the other hand, can mitigate risk.
But even a tight-knit family couldn’t protect Amy Cuzzola-Kern when she got stuck in prolonged grief. On a December morning in 2016, this social worker from Erie in Pennsylvania received a call from her father. ‘Something is wrong with your brother Chris. I can’t wake him up,’ he said. ‘I think he might be dead.’ She jumped into the car and rushed to her parents’ house, but it was too late. Chris, a sporty man who had just turned 50 that same year, had died in his sleep. The autopsy would later show that he had suffered a coronary artery blockage. Nobody had known, as Chris had been asymptomatic. His death struck the family out of the blue.
‘I knew he was dead, but I didn’t want to accept it,’ Amy told me during a Zoom call. ‘I was in major denial.’ Chris was her only sibling and her best friend. She had seen him every day since they were babies. With him gone, she ruminated about her role as a sister. Over the next two and a half years, Amy’s social life turned upside down. Before Chris’s death, she had been an energetic, sociable go-getter. After his death, she isolated herself and stopped spending time with her family and friends. When her husband asked her to accompany him to charity events, she refused.
‘I became a hermit,’ Amy says. ‘I rarely left the house. And when I did, I went for long walks. Alone.’ She chose routes that didn’t remind her of Chris. Out of fear she could meet common friends who would talk about Chris, she avoided going to bars or the movies. ‘In the grocery store, I’d pop in my earbuds, so I didn’t have to talk to anyone,’ she says. Both her denial and avoidance pattern are telltale signs of prolonged grief disorder. But she did not notice those signs at first.
It is true that bereaved mothers never recover from the loss of a child
What Amy did notice was her ongoing and overwhelming sadness, and she decided that two and a half years of suffering were enough. She told her general physician she was in a low mood all the time and asked for help. The doctor suspected a depression and prescribed her an antidepressant. ‘Six months into the treatment, you could have lit my hair on fire, I wouldn’t have cared. But it didn’t help at all with my grief,’ she explains. Because almost every psychotherapist ‘does grief’, Amy also added talk therapy to the mix. However, even combined with antidepressants, the treatment failed. That’s because, while depression is a mood disorder, prolonged grief is a stress disorder, akin to post-traumatic stress disorder (PTSD), and rooted in a different region of the brain.
Studies back up this experience. One, from 2016, found that the commonly prescribed antidepressant citalopram performed no better than a placebo. Some of the trial’s patients had simultaneously undergone a therapy specially tailored to prolonged grief disorder. The medication did, however, have a small positive effect on those patients who also suffered from classic depression. It improved only the depressive symptoms, not the grief-specific ones.
This might indeed explain why my mom felt a little better for a while when she, too, finally tried an antidepressant; she found that some depression lifted for a while, but her prolonged grief-specific symptoms didn’t subside at all. So, after trying several antidepressants, she gave up.
We often fought about her not wanting to try psychotherapy. I had moved out and started a job in a nearby city, but I kept offering to visit a psychotherapist with her. She turned me down with a barrage of rhetorical questions. ‘What good is a psychotherapist going to do? Does he know what it feels like to lose a daughter?’ There was no arguing with her. In her mind, this was her cross to bear, and she would die with it. There’d be no cure for ever healing a grieving mother, she said.
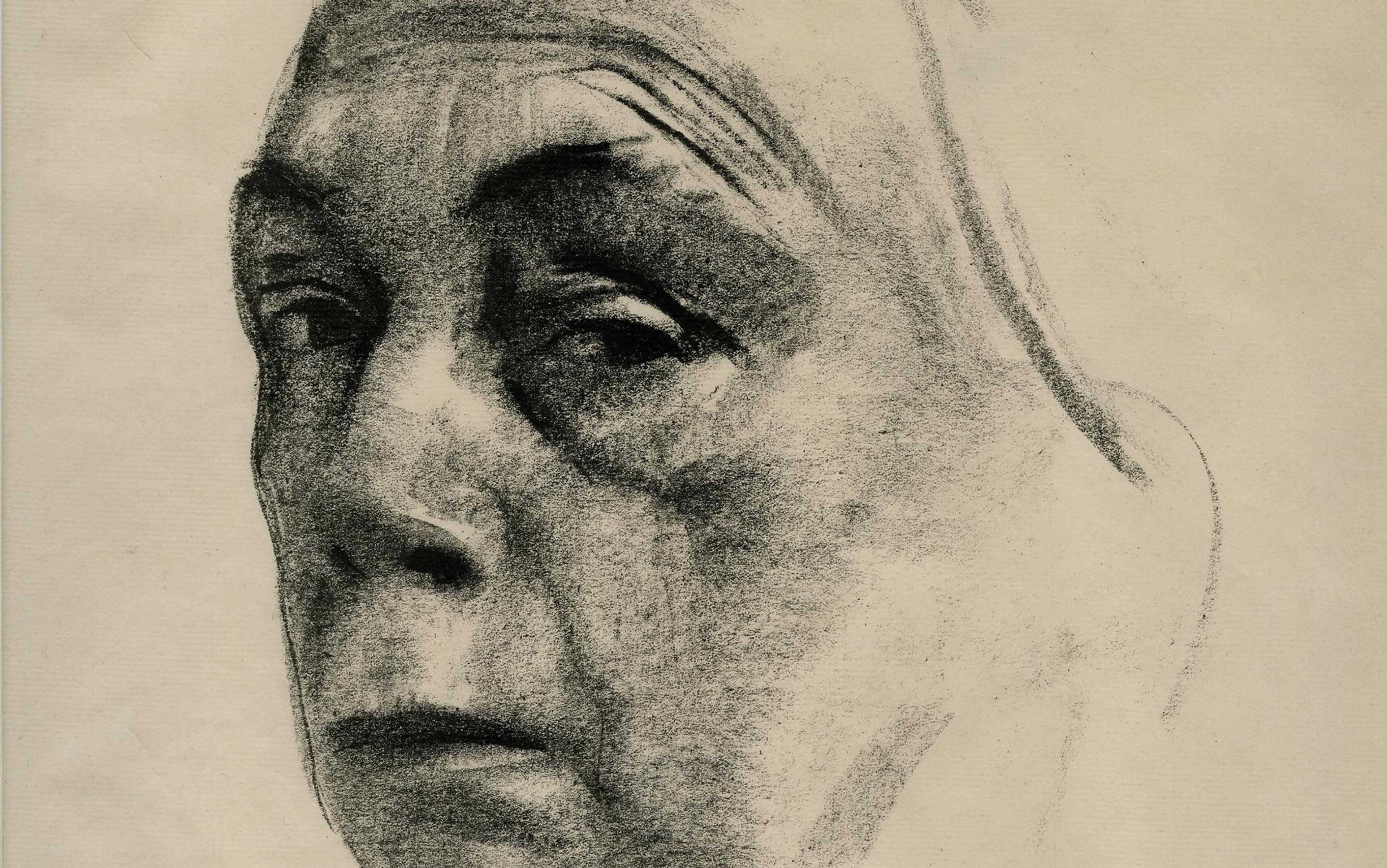
That latter part was right. It is true that bereaved mothers never recover from the loss of a child. A 2022 study shows that the experience changes their brain activity. Researchers at the University of California, Irvine showed grieving mothers photographs of their deceased children while observing their brains’ blood flow in an fMRI scanner. They found a particularly strong connection between two brain regions: the first, the amygdala, decides what’s important and manages anxiety. The second, the paraventricular thalamic nucleus, influences how we respond to long-term emotional memories. A feedback loop between the regions is especially triggering, sometimes even provoking the fight-or-flight response. The authors also found that severe grieving permanently lowered the mothers’ capability to learn, use language and manage their thoughts.
Neuroscientists have known for decades that grief affects the brain. Back in 2003, the clinical psychologist Mary-Frances O’Connor of the University of Arizona detected these changes using an fMRI scanner. She and her team interviewed eight participants to gather details of how the death had occurred. They also asked them for a photo of the deceased. The scientists then provoked grief reactions by showing the participants combinations of photos of the deceased and words like ‘funeral’ that reminded them of the death. The resulting fMRI scans show that a whole network of brain areas lit up, including the regions for processing, visualising and retrieving emotion-laden memories. A comparison with neutral words and photos showed no such activity.
Grief also alters the brain’s size. O’Connor pointed me to a Chinese study that found grieving people had a smaller left hippocampus. The seahorse-shaped brain area plays a crucial role in forming memories. Strikingly, one of its functions is verbal memory – which was impaired in the grieving mothers in the Californian study. Grief shrinks the brain area indirectly, as a result of too much stress. ‘What causes the hippocampus to shrink is an excess of the stress hormone cortisol,’ O’Connor says.
Another, equally prominent hormone sheds more light on how prolonged grief alters our brains. The ‘social hormone’ oxytocin is naturally released during breastfeeding and sexual intercourse, binding to receptors in the brain. ‘We believe that patients with prolonged grief disorder have less oxytocin receptors in their reward system,’ O’Connor says. In a recent study, she administered the hormone to patients via a nasal spray. It increased the activity in the same brain areas that are more active in grievers, so oxytocin is definitely somehow involved. But the hormone did not decrease the symptoms of grieving. So, a nasal spray curing prolonged grief won’t hit the market anytime soon.
However, another drug shows more promise. Researchers at Weill Cornell Medical College in New York City, led by the medical sociologist Holly Prigerson, argue that prolonged grief disorder can be classified as an addiction, since it involves the same reward pathways as alcohol or opioid addiction. That is why they are administering naltrexone pills to the participants of an ongoing clinical trial. Naltrexone is an opioid antagonist used to treat addiction. Prigerson and her team say that naltrexone takes effect faster than most antidepressants and is cheaper than other opioid antagonists like methadone. This would also help curb grief-related suicides.
Depression and grief have different neural pathways; grief is essentially a stress response
While the trial is not yet complete, Prigerson said in an email that psychiatrists report benefit from the approach. ‘Naltrexone in those with PGD [prolonged grief disorder] led to them venturing outside and having opportunities for new social connections,’ she wrote. The principle behind the treatment is based on reducing the continuous focus on the deceased person. Loosening this bond would open treated patients to new relationships.
O’Connor, meanwhile, prefers specialised psychotherapy to alleviate prolonged grief symptoms; naltrexone, she complains, is so broad it may hinder new attachments to others even as it eases the old. And, increasingly, those therapies can be found.
Despite three failed psychotherapies, Amy Cuzzola-Kern refused to give up. She kept scouring the web and newspapers to understand what she was suffering from, and to find help. By chance, she stumbled on an article that mentioned the Center for Prolonged Grief. Shear, its director, had developed an evidence-based therapy called prolonged grief disorder therapy (PGDT).
I too found the diagnosis and treatment by mere chance. I hadn’t been actively looking for an explanation of my mom’s condition any more. I had given up. Then, one June morning last year, an email announcing Shear’s new book chapter on PGDT popped up in my mailbox. As a journalist, I filed it under ‘story ideas’ and returned to it later that afternoon. A few pages in, my eyes widened: my mom ticked all the boxes. Here was my chance to finally understand what she had gone through. I needed to talk with scientists, scour studies and explore this disorder through my writing. It felt like this was the one last thing I could do for her. So I called Shear to learn how she had come up with the treatment and what it entailed.
Shear ’s 16-week programme, tapping the decades of prior research, acknowledges that depression and grief have different neural pathways, and that antidepressants could not help. Starting from the premise that grief is essentially a stress response, she reached out to Edna Foa, her friend and colleague. Foa had shown that prolonged exposure to a trigger was an effective therapy for another stress disorder, PTSD, and had trained Shear’s team of therapists in her technique. Today, Shear’s grief therapy involves exposure through techniques like imagery, imagining conversations with the deceased loved one, and identifying meaningful life goals.
Shear has also proposed diagnostic criteria for prolonged grief disorder; after much debate within the psychiatric community, her work and others’ led to official inclusion of the diagnosis in the DSM-5-TR in 2022. The new diagnosis helps patients find proper treatment, and also enables them to get grief therapy reimbursed by their insurance plans.
One of those patients was Amy Cuzzola-Kern. She couldn’t just sign up for the therapy, of course. Before taking her on as a patient, Amy’s therapist (a colleague of Shear’s) had to ensure that she did indeed suffer from PGD. Amy completed a questionnaire based on the ‘Inventory of Complicated Grief’, which itself is based on years of research into the field, with questions like ‘Do you avoid reminders that the person who died is really gone?’ Amy scored high enough on measures of pathological grief to qualify for a pre-treatment interview and, soon after, her weekly sessions began.
Amy badly wanted to undergo therapy to stop her suffering, but she also felt a lot of resistance. ‘I was worried that I would forget Chris’s memory,’ she says. This ambivalence is typical of prolonged grief, which is why some researchers call it ‘bittersweet’. Recalling memories may be painful, but for many patients they are the only relationship they have left with their lost loved ones. As much as they want their symptoms gone, they cling on to their memories. Patients fear that therapy will erase those memories. That is the reason, Shear tells me, why many PGD sufferers put off seeking help for years.
But the opposite is true, she says: ‘PGDT does not extinguish patients’ memory of the deceased person, but rather, helps them accept the loss and restore their own wellbeing.’
Shear’s therapy uses a conglomerate of therapeutic techniques to tackle the different symptoms from which patients suffer. In the first session, every patient is asked to start writing a grief-monitoring diary. It is a five-minute at-home exercise, in which Amy had to record when her grief peaked and what had triggered it.
One exercise was to revisit his death in her mind, an exposure technique used by PTSD sufferers
Then, during the therapy sessions, they talked about her diary entries, the triggers, and about the ways she had coped with her grief. Shear calls some of these coping mechanisms ‘derailers’. They are often initially helpful to reduce the stress level, but eventually all of them turn against the patients. Common derailers include isolation, guilt and self-blame.
In fact, Amy was derailed by more than isolating at home and turning down all social events. She also tended to ponder ‘What if?’ scenarios. The night before Chris’s death, the family had gone through a tough day. Amy and her brother had accompanied their mom to Cleveland where she underwent chemotherapy. When they came back, Chris was very tired and went to bed early at his parents’ house, where he was staying to help with their mom’s frequent injections. Although Amy had talked to Chris before saying goodnight, counterfactual thoughts crept into her mind afterwards. Thoughts like: ‘He looked really tired, maybe there was something else going on with him. I should have asked him.’
All this reminded me of a thought that has been lingering at the back of my mind for the past 30 years. My mom and I never talked about it. Ever. It was taboo. On that January evening, my sister Claudia had not gone to the grocery store to buy something for herself. In fact, she had not wanted to leave the house at all. Instead, my mom had sent her out because she had run out of her favourite hairspray. Nobody could have foreseen what would happen, but nonetheless: hadn’t my mom been consumed by guilt?
‘Patients often experience thoughts like this. We call it caregiver’s self-blame,’ Shear says. ‘When a child dies, regardless how, they experience a feeling of failure as a caregiver. It is irrational, but people go through all sorts of hypothetical scenarios, like If I had sent her out 10 minutes later, nothing would have happened.’ The more counterfactual thoughts of this kind somebody experiences, the higher the severity of their prolonged grief, a study from 2021 shows.
The therapy does not have one specific technique to extinguish guilt. But Amy’s counterfactual thinking dissipated once she started accepting Chris’s death. One key exercise to achieve that was revisiting his death in her mind, an exposure technique that PTSD sufferers use to come to terms with trauma. Amy’s therapist asked her to tell him the story of how Chris died. She had to record it on her phone and listen back to it at home, every day. In the ensuing sessions, she had to re-tell the story and re-record it. With every new version, the narrative became slightly more detailed. This helped anchor the events in reality. Over time, it also dispelled her fear of losing her memories of Chris.
At the beginning, the task was tough, so her therapist asked her to reward herself with little pleasures. It could be anything, he said, a piece of chocolate or a glass of wine. Amy found none. But then she went on a family holiday in Florida. As she was floating in the pool, listening to podcasts, she learned again to carve out quality time for herself. Slowly, she began to practise more self-care. Her therapist also started working with her on her avoidance behaviour. Instead of popping in earbuds, Amy started having little conversations with the people she met at the supermarket. The closer her therapy came to its end, the more Amy came around.
Before the therapy, Amy had lost her sense of her future and her life goals. Her therapist had to force her to write down an aspirational goal. ‘That was really, really hard,’ she recalls. But eventually, she found one. When the therapy ended, Amy pursued a masters in social work at Shear’s Center for Prolonged Grief. She finished it last year and now wants to help other bereaved people. ‘We’re not meant to grieve alone,’ she says. ‘When somebody close suddenly dies, you need a whole posse of people to help you. For those who have nobody, that is the therapist.’
I wish that I could end this piece writing that my mom came around, too. But she didn’t. Shortly before the pandemic hit, she received a diagnosis. Lung cancer, terminal. Had it not been hopeless, she would have made good on her promise and refused treatment. Despite pandemic rules, a nurse snuck me in to the ICU so I could say goodbye. My mom was unconscious. I cried because she was about to go. But I also cried knowing that she had spent more than half of her life grieving. I now know it didn’t have to be that way. Her condition has a name. It can be treated. It could have been treated. If only.