A century ago, invasion of a beating heart was off limits to doctors. To pass through its pulsating walls, with scalpel or otherwise, was seen as an uncharted expedition where risk of death for the patient was exponentially high. Theodor Billroth, an early innovator of modern surgery, allegedly remarked that: ‘No surgeon who wished to preserve the respect of his colleagues would ever attempt to suture a cardiac wound.’
And so, early attempts at surgery on a living heart were conducted in situations where recklessness was deemed appropriate. In 1896, the first successful suture of the heart was performed on a stabbing victim who would have died if his surgeon, Ludwig Rehn, had cared more about gaining the respect of his colleagues. While this early success inspired confidence in the pioneers of heart surgery, progress in cardiac surgery was dismally slow. Bypass procedures – where new pathways are surgically created when arteries are blocked – were not trialed until the mid-20th century. Astonishingly, cardiothoracic surgery, where lungs and chest are also involved, is seen as one of the most technically advanced fields of medicine, despite a majority of these advancements having been made over the relatively brief span of half a century.
That such prudence was paid to the heart is reflective of more than just the physiological difficulty of operating on the powerful muscle responsible for circulating our most vital fluid. It also represents deference to our passions and desires. When a lover betrays us, we are ‘heartbroken’. Fits of rage and anger are marked by our hearts ‘pounding in our chest’. When a potential mate flirts with us, we experience a ‘flutter in our breast’. Such psychological and sentimental attributions to the heart raised its significance beyond its circulatory function, and established a taboo that was cultural, in addition to anatomical.
Adding to this taboo is the emphasis placed on the heart by religious images and texts. The first depiction of Jesus that I can recall is from my devotedly Catholic grandmother’s house. In it, the bearded figure stood with a glowing heart protruding from the centre of his chest. This ‘sacred heart’ is said to represent, for some, the greatest love imaginable – the love that Jesus had for the whole of humanity. Most interpretations of the Hebrew bible understand the heart to be the seat of one’s emotive and intellectual states, both of which are necessary to establish a connection to God and their community. One can find similar interpretations in the Quran, in which the heart is described as the centre both of one’s emotions and of one’s ability to uncover truths. Citta, sometimes translated as ‘heart-mind’, is a central part of certain Buddhist meditative practices. Hanuman, a Hindu god of strength, courage and self-discipline, is often depicted with his chest torn open, revealing the goddess Sita and the god Rama presiding within his heart – a symbol of his loving devotion to them.
Against this immense medical, cultural and religious backdrop, we can turn our attention to the early 20th-century German physician Werner Forssmann. Perhaps the best summation of Forssmann’s legacy is the title of his profile in the journal Clinical Cardiology – ‘Werner Forssmann: A German Problem with the Nobel Prize’ (1992). Werner’s problematic nature can be understood through his proclivity towards self-experimentation, which seems to have begun early in his career. His doctoral thesis, which examined the effect of liver consumption on human blood, consisted of studying the blood chemistry of those who drank a litre of concentrated liver broth. Forssmann recruited a small group of students to help with his experiment; they would drink the liver broth every day for a fixed period, and then have their blood chemistry examined. However, Forssmann, who had an eclectic test-it-on-oneself drive, decided to also take the liver broth and measure the effects that it had on his own blood chemistry. While such a low-risk exercise in scientific curiosity is not a cause for major ethical concern or worry, it forebodes a much more ethically worrisome self-experiment.
The suggestion that Forssmann conduct his experiment on animals did not satisfy his drive for innovation
One summer afternoon in 1929, during the customary siesta hour of a small regional hospital, Forssmann carried out another self-experiment that had been on his mind for quite some time. The inspiration behind this experiment came from a 19th-century medical text by the French physiologists Jean-Baptiste Chauveau and Étienne-Jules Marey. The book contained an illustrated diagram depicting a man holding a tube that had been inserted into the neck of a horse. This tube had been led down the horse’s jugular vein and was illustrated as being situated in the right ventricle of its heart. This image piqued Forssmann’s curiosity, and he began to wonder if a similar procedure could be successfully performed on a living human being – albeit with some adjustments.
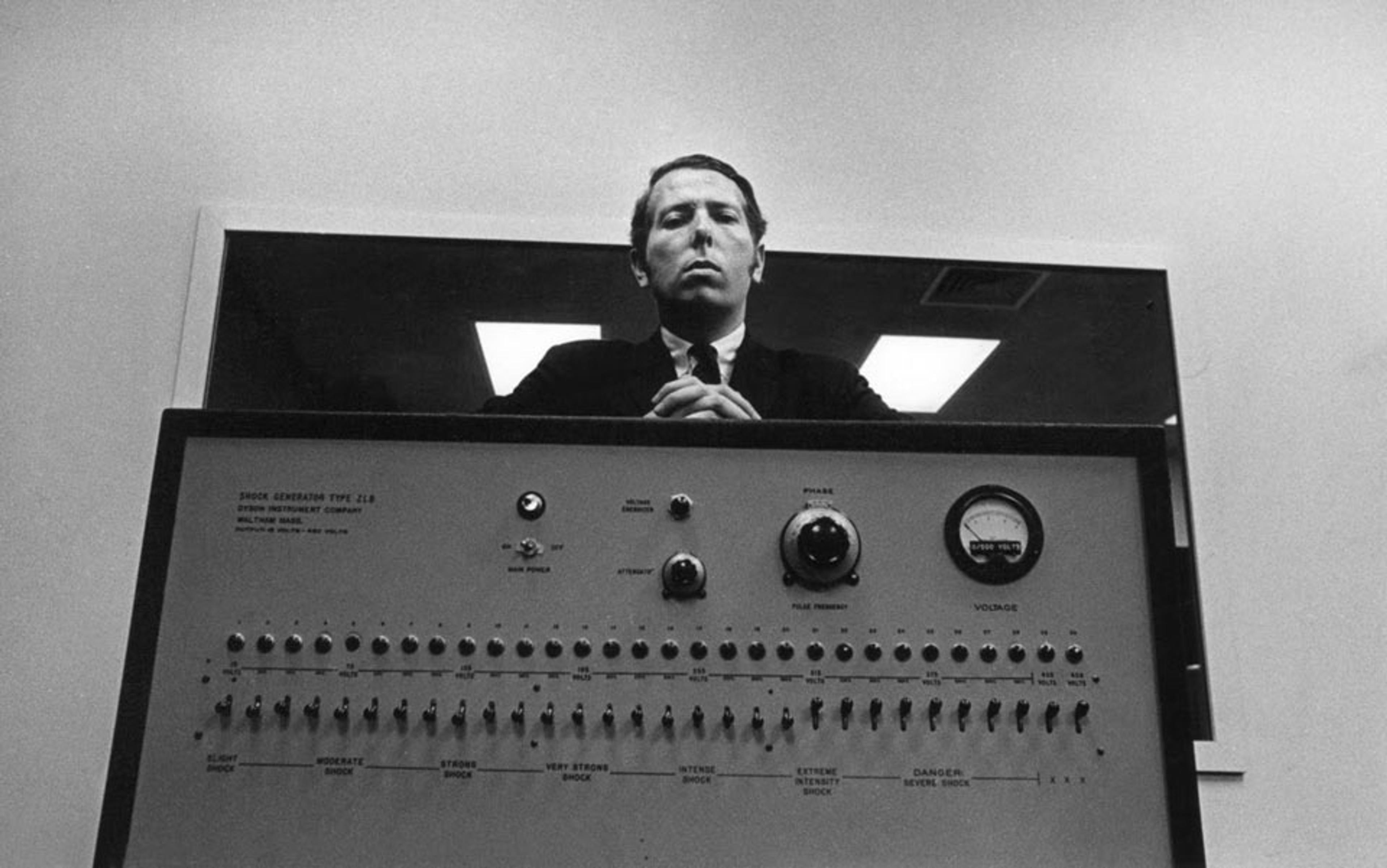
An X-ray image documenting cardiac catheterisation, showing the catheter extending into the right atrium. From ‘Die Sondierung des Rechten Herzens’ (‘Probing of the Right Heart’) by Werner Forssmann, Klinische Wochenschrift, November 1929.
Namely, the jugular vein in the neck would be an inappropriate route for accessing a human heart because it carried the risk of developing an air embolism – a condition in which a pocket of air builds in a vein or artery and prevents blood flow, potentially a prelude to a fatal heart attack or stroke. Instead of the jugular, Forssmann thought it more appropriate to use the veins located in the pit of the elbow; these veins were already safely used for intravenous injections.
So, Forssmann developed the following procedure: a patient would lift their arm so that it was parallel to the floor, the vein in their elbow would then be accessed via a small incision and a catheter line would slowly be led into the vein, and then, using the guidance of an X-ray fluoroscope, the line would be carefully led into the left ventricle of the patient’s heart.
Forssmann did not originally plan to conduct this experiment on himself. He had pitched the idea of performing this experiment on a patient to his supervisor, Richard Schneider. However, despite Forssmann’s enthusiasm, Schneider was unmoved by the proposal. The reason for Schneider’s rejection was quite practical in nature: he could not permit novel research to be conducted in a hospital whose facilities could not accommodate it. Though he imparted to Forssmann that such research would have to take place in a larger, more established facility, he did not wish to entirely chill Forssmann’s scientific curiosity. Schneider therefore suggested that Forssmann conduct his experiment on animals. However, this suggestion did not satisfy Forssmann’s drive for innovation. After all, the experiment had already been performed on a horse; there would be no novelty in repeating it on another animal.
Irrespective of Schneider’s judgment on the matter, Forssmann’s experimental urge remained undeterred, and he began to gather the necessary resources.
He determined that he needed the cooperation of at least one other person: Gerda Ditzen, the department’s operating room nurse, and so in charge of sterilising the surgical equipment. Forssmann warmed up Ditzen to his plan by persuading her of the groundbreaking medical progress such an experiment could unlock. As a pump, the heart functions by using pressure to draw in and expel blood. If clinicians were able to measure the pressure that the heart uses, they would be able to assess how well a patient’s heart was functioning. At the time of Forssmann’s experiment, relatively little was known about the physiological causes of heart failure or other cardiac disorders. Assessing functioning by measuring and recording the various pressures of the heart and surrounding veins and arteries could be helpful in diagnosing or discovering new cardiac disorders. Establishing access to the ventricles of the heart, however, would be a necessary first step in making these discoveries. If Forssmann’s experiment worked, clinicians could be granted access to the inner workings of a beating heart with a minimally invasive procedure.
The thrill of being part of this important medical discovery allowed Ditzen to see past any scruples she might have had regarding the experiment. She agreed to help Forssmann with the procedure and would provide him with the sterilised equipment. However, Ditzen was operating under the seemingly logical assumption that Forssmann would perform the experiment on her, not on himself.
And so, on that summer afternoon, the pieces of Forssmann’s plan fell into place. The equipment was sterilised, the rest of the hospital staff were taking their siesta, and Forssmann and Ditzen found themselves alone together in the operating room. Forssmann explained to Ditzen that, due to the possibility of her fainting after the administration of Novocain, she would need to be supine for the procedure. So, Ditzen lay down on the operating table and offered up her arm to Forssmann. He then told Ditzen that he would also need to strap her to the table in order to prevent her from rolling off in case she were to lose consciousness. Ditzen agreed with Forssmann’s reasoning and allowed him to restrain her to the table. Ditzen was essentially tied up.
He was reasonably certain he could safely lead a catheter up to his shoulder, before the vein bent towards the heart
In truth, such preparations simply ensured that Ditzen would be able to neither see nor prevent Forssmann’s actions. Once out of sight from Ditzen’s view, Forssmann began to anaesthetise the pit of his own left elbow with Novocain. He then went to Ditzen’s side and pretended to iodise her own arm in order to sterilise it for the procedure. Such play-acting bought Forssmann the time necessary for his own anaesthetic to take effect. Once he determined that his arm was sufficiently numbed, he began his self-experiment by making an incision that allowed access to a vein located in the pit of his left elbow.
Much like the highways leading from the suburbs and into the heart of the city, our veins are the route that our blood takes back to our own hearts. Like highways, veins vary in size and structure. Some veins take a complex and winding path to the heart, whereas others are more or less straight shots. For instance, the antecubital vein, which Forssmann had just accessed, leads straight up the arm, bends slightly at the shoulder, and then flows down directly into the heart. Since this vein leads straight up the arm, Forssmann was reasonably certain that he could safely lead a catheter – a small rubber tube with a metal tip – up to his shoulder, right before the vein bent towards the heart. Once the catheter’s tip reached his shoulder, he would need the visual assistance of an X-ray fluoroscope to guide him the rest of the way to the heart. The fluoroscope, a machine that provides a real-time X-ray image of the body, would allow him to determine if his experiment was headed for disaster; it would show if the catheter’s tip had internally punctured his vein – which would require immediate medical attention – or if the catheter had gotten stuck, meaning it would have to be pulled from his arm.
To reach the machine, which was in the hospital’s basement, Forssmann decided that he would have to free Ditzen from the table for her assistance. Now releasing her arm straps and loosening her leg restraints, he tersely stated: ‘There we are, it’s ready now. Please call the X-ray nurse.’
Ditzen eventually arose from the table and out of her confusion, realising that Forssmann had essentially tied her up while he performed the procedure on himself. Understandably upset, she began to yell at him. Nevertheless, she soon grasped the gravity of the situation: Forssmann had a uterine catheter hanging out of the pit of his elbow and could be in grave danger. Such a concern provided the impetus necessary for Ditzen to further comply with Forssmann’s requests.
She phoned the X-ray department to get them ready for Forssmann to come down. After all, it was still the siesta hour, and so the department would be unprepared to accommodate an emergency fluoroscope without some notice in advance. After the call, Ditzen seemingly remained concerned for Forssmann’s wellbeing, or perhaps she simply had the curiosity to see if the experiment would succeed, and so she accompanied him downstairs to the X-ray department. When they arrived, the X-ray nurse, named Eva, placed Forssmann behind the fluoroscope and began to position it so that they could locate the catheter’s tip.
Just then, adding to the absurdity of the scene, Forssmann’s colleague, an internalist named Peter Romeis, burst into the X-ray room and shouted: ‘You idiot, what the hell are you doing?’ He then tried to yank the catheter from Forssmann’s arm, fearing that Forssmann would gravely injure himself if he proceeded with the experiment. Forssmann was able to fend off Romeis with ‘a few kicks on the shin’.
Once things settled down, Forssmann ordered a mirror be placed in front of the fluoroscope screen so that he could see where the catheter was in his vein. He observed that the catheter’s tip sat at the top of his shoulder. So far, physiologically speaking, the experiment was going as planned. With the mirror positioned in front of him, Forssmann used the fluoroscope to witness the catheter’s slow advance as he carefully pushed it up his arm. After sending 30 more centimetres of catheter line into his arm, the fluoroscope showed that the catheter’s tip sat inside his heart’s right ventricle. He had done it. He had entered into his own beating heart.
Forssmann had taken an important step towards dispelling the cultural taboos surrounding the heart
The significance of this moment is two-fold. Physiologically, Forssmann had shown that the living heart could now be explored via a catheter with no physiological repercussions or advanced surgical techniques. The procedure was minimally invasive, requiring only a small incision to access a vein. What’s more, Forssmann was able to access his heart using only a local anaesthetic to numb the site of the incision, which meant that no heavy sedation or general anaesthetic was required. This is important because general anaesthetic often cannot be tolerated by patients with conditions that reduce their heart function.
In addition to this physiological significance, Forssmann had taken an important step towards dispelling the cultural taboos surrounding the heart. While modern medicine was already on a path to demystify the heart by showing its primary function was the circulation of blood via rhythmic electrical waves, popular attitudes of the heart still regarded it as a psychologically significant organ responsible for passionate desires. But Forssmann’s experiment showed that medicine could access the heart in a manner that posed no risk to the organ held in such high regard.
At first, Forssmann’s supervisor, Schneider, was astonished by both the recklessness and the results. But soon more practical concerns, including how to publish, entered their minds. While Forssmann’s experiment was scientifically compelling, in that it uncovered the possibility of reaching a still-beating human heart, Schneider believed that scientific curiosity alone would not help journal editors to see past the ethical concerns. He hoped that, if only Forssmann could show some immediate therapeutic benefit, an editor would overlook the questionable ethics involved.
Eventually, Forssmann would find a therapeutic use for the procedure: by establishing a catheter line to the heart, physicians could administer certain drugs that proved more effective when administered via the line. With this clinical use established, Forssmann wrote up a manuscript and sent it to one of the most esteemed German medical journals. To his surprise, it was accepted, and even contained an X-ray image of Forssmann’s own heart with the catheter tip resting inside his right ventricle.
Yet the true clinical relevance of Forssmann’s experiment would not be realised until a decade later, when his article came to the attention of the physician André Cournand. Generally speaking, the functions of the heart can be split into right and left: the right side is responsible for drawing in blood that is low in oxygen and propelling this blood into the lungs where it is then oxygenated. This oxygenated blood is then drawn back into the heart and propelled to the rest of the body by the left side of the heart.
This drawing in and propelling out of blood – the heart’s essential function – can be assessed by measuring the various pressures within the heart and the surrounding veins and arteries. And, it goes without saying, without the cardiac catheterisation pioneered by Forssmann and utilised by Cournand and his colleague Dickinson Richards, a majority of cardiac conditions would go undiagnosed and untreated today. Currently, cardiac catheterisation is one of the most commonly performed medical procedures. In the United States alone, more than 1 million cardiac catheterisations are performed each year.
Cardiac catheterisation is also used for angioplasty, the most frequently used procedure in the event of a blocked coronary artery. During the procedure, a catheter is inserted into an artery located in either the arm, leg or groin. Then, with the assistance of a real-time X-ray (ie, a modern-day fluoroscope), the catheter is led up the artery until it reaches an area close to the suspected blockage. A contrast dye is then sent through the catheter and into the artery to identify the exact location of the blockage. The catheter is then led to the blockage and a small balloon is inflated to stretch the artery, which then amends the blockage. In some cases, a small wire mesh – a cardiac stent – is placed in the artery to keep it unblocked. Coronary angioplasty is crucial in preventing or treating heart attacks, one of the leading causes of death.
Given all this, it can be said that the experiment Forssmann conducted on himself spurred developments in cardiology that would go on to save and extend countless lives. It’s only fitting that, along with Cournand and Richards, he was awarded the Nobel Prize in Physiology or Medicine in 1956.
His colleagues held him in high regard. In Clinical Cardiology, Forssmann is remembered as ‘a great character, gifted surgeon, and pioneer in cardiology’. In the European Heart Journal, his experiment is characterised as having ‘immense significance in paving the way for a monumental leap forward in cardiovascular care’ and ‘an outstanding act of selfless courage’. In the preface to Forssmann’s aptly titled memoir Experiments on Myself (1974), his fellow Nobel awardee Cournand describes Forssmann as a man ‘full of resources and will power, and endowed with physical courage’.
Such a warm reception for self-experiment among clinicians is not surprising. At the turn of the 20th century, the US Army physician Walter Reed was sent to the newly occupied US colony of Cuba. Reed’s task was to study the tropical diseases that impacted soldiers during the recently concluded Spanish-American War. In particular, he was to investigate how yellow fever spread. Over the course of the three-month war, fewer than 400 US soldiers died in combat and more than 2,000 soldiers died from yellow fever infections. While the prevailing theory was that small particles, called fomites, where responsible for the spread of yellow fever, another theory proposed that mosquitoes carrying a particular pathogen were responsible for the disease. Reed’s task was to determine, once and for all, what exactly caused yellow fever.

Jesse William Lazear with his one-year-old son. Johns Hopkins University/Getty
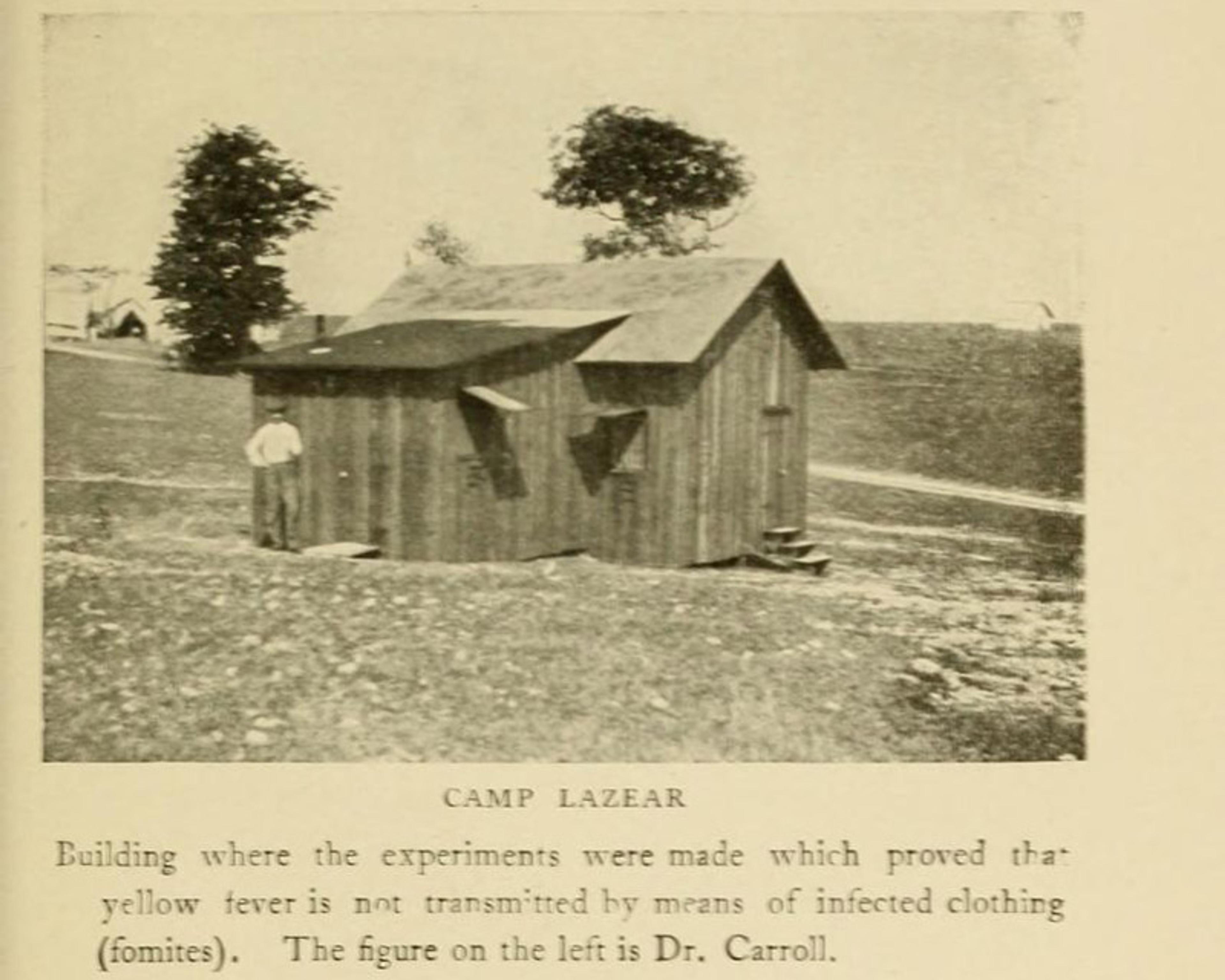
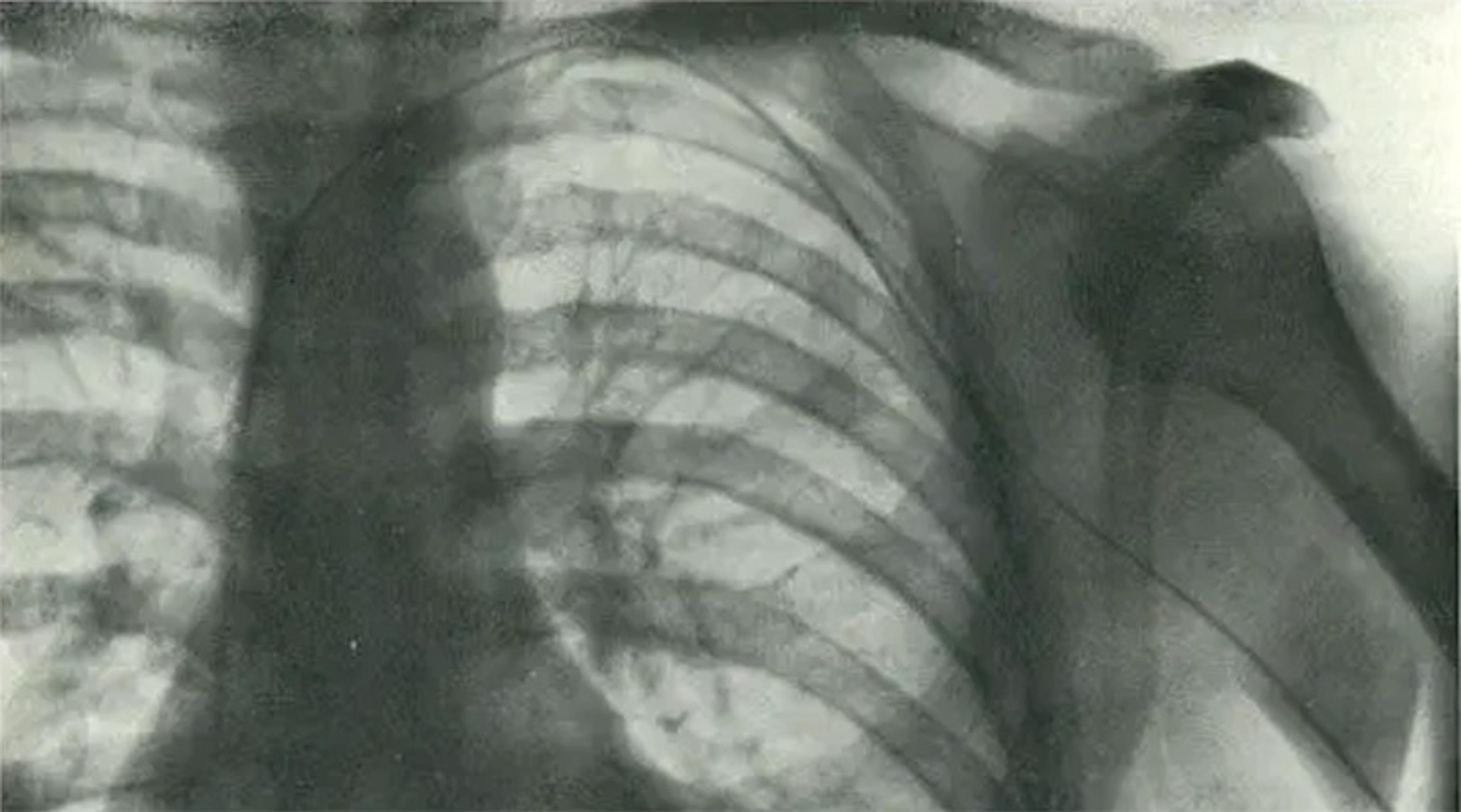
Experimental hut at Camp Lazear, Cuba. Wellcome Images
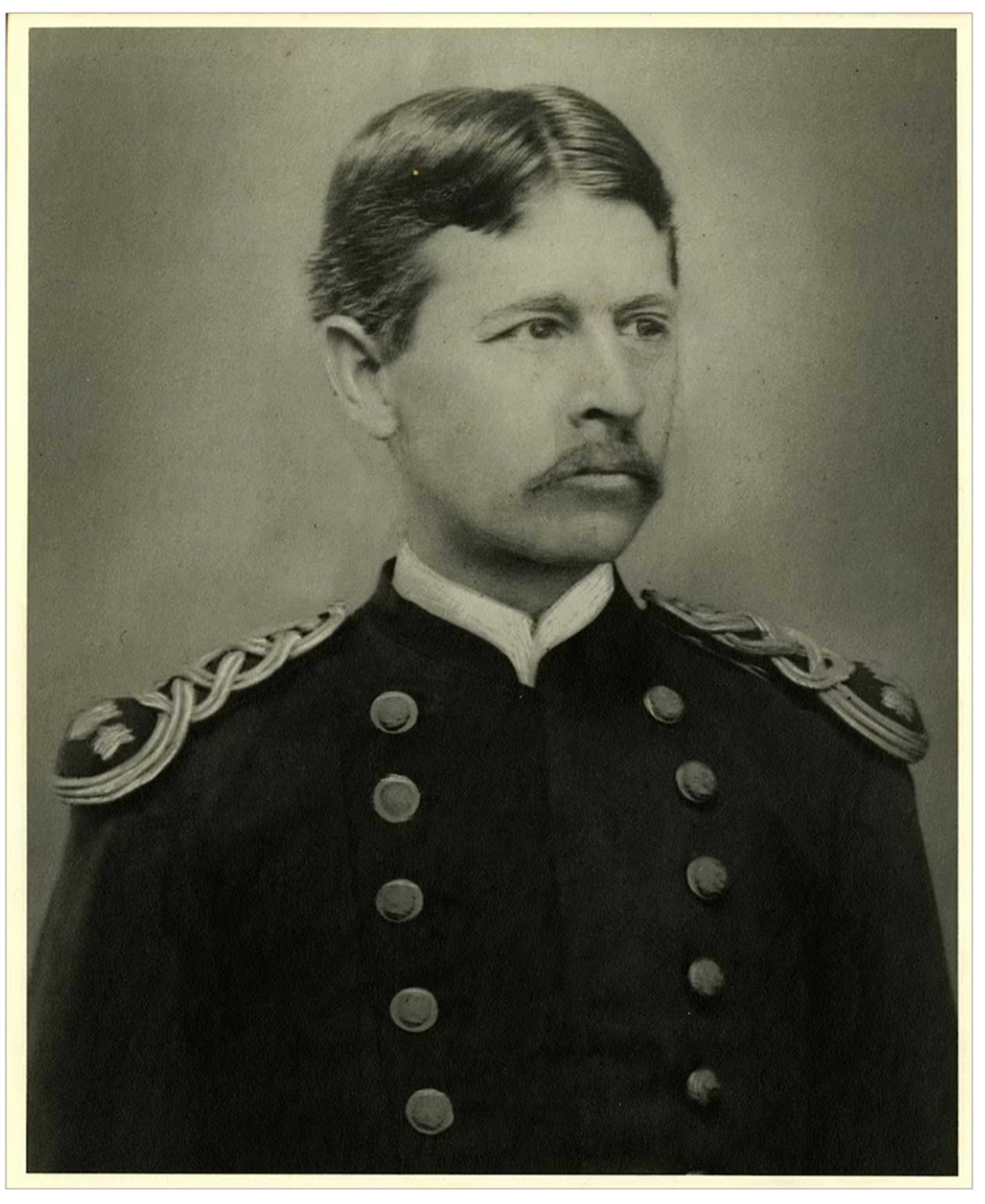
Walter Reed, c1900. Courtesy the Department of Defense
Along with his colleagues Jesse Lazear and James Carroll, Reed had tried to infect various animals with yellow fever, but these attempts were unsuccessful. Lacking an animal analogue on which they could conduct experiments, Reed, Lazear and Carroll determined that the only possible way to truly test the hypothesis that yellow fever was spread by mosquitoes was to use human subjects. The proposed experiment they came up with was quite rudimentary by today’s standards: a human subject would be bitten by a mosquito that was thought to be a potential carrier of yellow fever. If the bitten subject developed yellow fever, it would be evident that the mosquitoes were a vector for the disease. If not, it would be more likely that fomites were the cause for the disease.
Lazear allowed himself to be bitten by his mosquitoes and waited to see if it would result in an infection
Reed had gone to great lengths to calm the ethical worries that persisted around exposing human subjects to potentially deadly virulent matter. He drafted what is perhaps the first instance of a written consent document explaining the risks of participating in the proposed research. Nevertheless, the research board decided that, due to the dangerous nature of the experiment, they themselves should be among the first volunteers. That way, if the experiment did prove fatal, they would bear the burden of this risk.
In August 1900, Lazear, himself a member of the research board, began to raise a batch of mosquitoes from their larval stage, ensuring that he had fresh, uncontaminated mosquitoes. He then had this batch fed on a person with an active yellow fever infection. To test whether this batch, or any mosquito, could pass on the infection, Lazear allowed himself to be bitten by one of his mosquitoes and waited to see if the bite would result in an infection. When no signs of infection came, Lazear assumed it safe to allow other volunteers to be bitten by the mosquitoes. None of the volunteers developed an infection, and so the other research board member, Carroll, allowed himself to be bitten.
At this point, the evidence had pointed to mosquitoes not being a vector for the disease. So, it came as a surprise when, a few days after being bitten, Carroll developed symptoms of yellow fever. Dismayed at the possibility that mosquitoes could be the vector for the disease, Lazear hastily subjected a soldier, Private William H Dean, to a bite from one of his yellow fever-fed mosquitoes, to determine if they truly did carry the pathogen causing the disease. The soldier came down with the disease, which all but confirmed that mosquitoes were the vector. After this discovery, Lazear was subjected to another bite from an infected mosquito. While it is unclear whether Lazear allowed himself to be bitten or whether it was accidental, this bite would have fatal consequences. He developed yellow fever, as was to be expected, and died a week later from the disease.
Like Forssmann’s, Lazear’s self-experiment is viewed with reverence. He is enshrined in the ‘Sacrifice for Freedom’ stained glass window at the War Memorial Chapel of the Washington National Cathedral, which displays his self-experiment alongside a depiction of Jesus’ crucifixion.
Interestingly, Lazear’s legacy of self-sacrifice influenced the course of modern research ethics and its stance towards self-experimentation. The fifth article of the Nuremberg Code (1947) – a document that many regard as foundational to modern research ethics – states that:
No experiment should be conducted where there is an a priori reason to believe that death or disabling injury will occur; except, perhaps, in those experiments where the experimental physicians also serve as subjects.
This allowance of self-experimentation stems from an earlier working draft of the Code, which states that:
[I]t is ethically permissible for an experimenter to perform experiments involving significant risks … if he considers the solution of the problem important enough to risk his own life … such as was done in the case of Walter Reed’s yellow fever experiments.
And so, it appears that modern research ethics has carved out a unique allowance for self-experimentation. It is condoned, perhaps even endorsed, in cases where there persists an enormous risk to one’s wellbeing but also an enormous benefit to society.
This ethical allowance, even reverence, towards self-experimentation continues into the present day. In 2005, the Australian physician Barry Marshall and his colleague J Robin Warren were awarded the Nobel Prize in Physiology or Medicine for research examining the relationship between Helicobacter pylori (H pylori) and the development of peptic (ie, stomach) ulcers. These ulcers occur within the lining of the stomach and can cause a sharp, intense pain along with internal bleeding resulting in bloody stool or vomit. Through years of research, Marshall and Warren were able to show, definitively, that H pylori infections could cause peptic ulcers.
Marshall’s choice to conduct a self-experiment was crucial to shifting the paradigm
But, initially, Marshall and Warren’s hypothesis received a lukewarm reception within the medical community, which held that ulcers were caused by stomach acid due to psychological stress. Finally, to get a fair hearing in the face of disbelief, Marshall took matters into his own hands. In 1984, he had an endoscopy to confirm that he was not infected with H pylori. Then he drank a solution that contained two pure cultures of H pylori: essentially a megadose of the bacteria. Marshall knew that H pylori was slow growing and so he suspected that he would have to wait for months, maybe even years before he developed a peptic ulcer from the bacteria. It came as a surprise, then, that Marshall came down with a case of severe gastritis – a precursor condition to peptic ulcers – five days after consuming his bacteria-rich concoction. This made it all but certain that the bacterium was responsible for his gastritis.
After completing a course of antibiotics to treat his infection, Marshall and Warren published the results of Marshall’s self-experiment. This publication started to solidify the paradigm shift regarding the cause and treatment of peptic ulcers; the acid hypothesis slowly faded into the background as studies began to confirm that H pylori was the culprit for most cases of peptic ulcers.
Marshall’s self-experiment, like Forssmann’s or Lazear’s, is looked upon with praise. The award ceremony speech for Marshall and Warren’s Nobel Prize highlights Marshall’s self-experiment, depicting it as a necessary step for their research. Such praise also extends into the realm of medical ethics: the American Medical Association Journal of Ethics presented Marshall and Warren with a Virtual Mentor Award for being ‘exemplary role models in medicine’. Many profile articles, both in scholarly and popular media, have been written about Marshall, often highlighting his choice to conduct a self-experiment so crucial to shifting the paradigm regarding the underlying cause of peptic ulcers.
Logically speaking, it’s hardly surprising that our modern research-ethics environment has failed to find fault with self-experiments. Many of the current debates within research ethics centre around preserving the autonomy of research participants. For instance, a constant point of debate concerns how much information is necessary for research participants to be able to make an informed, autonomous decision regarding whether they want to participate in a research project. Some argue that providing only a minimal amount of information – such as risks, benefits and information about a research procedure through a written document – suffices in informing the potential participant about the research. Others say that a more detailed consent process, possibly involving a one-on-one, in-depth discussion that covers the research’s purpose, risks, benefits and procedure with each potential research participant, is required.
Such debates become non-issues when the researcher and research subject are one and the same. After all, the researcher who designs the experiment knows why the experiment is being done, what benefits it may have, and the potential risks that might come from undergoing such an experiment. If there would be anyone able to make a truly informed decision about whether they want to participate in the research, it would be the researcher who designed the experiment.
Another ethical concern seemingly side-stepped by self-experimentation is that of establishing a favourable risk-benefit ratio. The Belmont Report (1979), understood to be the central ethical doctrine for research conducted in the US, highlights that ‘benefits and risks must be “balanced” and shown to be “in a favourable ratio”.’ Generally, this means that research must be designed in a manner that assures participants face only the minimal necessary risks and that even these are aligned with an equal or greater benefit. In the case of self-experimentation, such concerns seem to be more a matter of personal prudence rather than an ethical consideration of another’s wellbeing.
In fact, using the principle of autonomy that dominates our present research ethics environment, it could be argued that it is unethical to encroach upon those who wish to conduct a medical experiment on themselves. What right would anyone have in preventing someone from doing an experiment upon themselves that progressed science or bettered humanity?
But does celebration of the self-experimenter overlook requisite concern for them? Have we become so excited by the bravery displayed in sacrificing one’s wellbeing for the advancement of a humanistic endeavour such as medicine that we have overlooked a basic ethical responsibility to do one’s own self no harm?
At least Forssmann was unwilling to perform the potentially dangerous experiment on Ditzen
In Forssmann’s case, the ethical concerns start with his treatment of Ditzen. There are many ways Forssmann disrespected Ditzen as a person. First, he used her; he stoked her curiosity and excitement regarding groundbreaking research only so that she would agree to sterilise a set of instruments for Forssmann to use. Second, he deceived her; she was under the impression that the experiment would be conducted on her, and Forssmann allowed her to carry on with this impression despite him having no intention of performing the experiment on her. Third, and perhaps the most blatant form of disrespect, he restrained her; he strapped her to the operating table, meaning that she was essentially being tied up and restrained against her will.
However, despite these instances of disrespect, it should be noted that at least Forssmann was unwilling to perform the potentially dangerous experiment on Ditzen. The reasons for this decision could be numerous, as Forssmann offers us no explanation as to why he decided not to experiment on Ditzen despite her willingness. Yet, a parsimonious explanation for Forssmann’s decision is that he had respect for Ditzen’s wellbeing and personhood. That is, Forssmann recognised that the experiment was not free of risk or adverse consequences: such an experiment had never been conducted in humans and thus could come with numerous unforeseen dangers. What’s more, the experiment was being conducted during what amounted to the lunch hour at a small regional hospital; if things did go awry, it was uncertain if help could arrive in time.
Needless to say, subjecting someone to a risky and hastily planned first-in-human experiment amounts to disrespecting their personhood. The second formulation of Immanuel Kant’s categorical imperative – sometimes referred to as the ‘humanity formula’ – serves as the moral basis for the notion that research needs to consist of respect for persons. In its entirety, the formula reads:
Act in such a way that you treat humanity, whether in your own person or in the person of any other, never merely as a means, but always at the same time as an end.
Generally, this is taken to mean that a researcher should not treat human subjects as merely instruments to obtain some research goal, but rather recognise that they are persons who are able to make their own rational choices to achieve their own unique goals. More often than not, this interpretation of the humanity formula is simplified to the following claim: research participants have the right to consent to and voluntarily withdraw from a research project. While this interpretation of the formula is perhaps sufficient in respecting a participant’s autonomy, it does not capture Kant’s important claim that human beings are particularly unique in that they possess an inherent moral value.
Kant’s humanity formula distinguishes between objective and subjective ends. Subjective ends, which Kant sometimes refers to as material ends, are things that have value only within the unique material contexts of a person’s life – a new car, say, or a job promotion. Objective ends, on the other hand, have value irrespective of someone’s unique desires or individual contexts. For Kant, the prime example of an objective end is a person, since they retain their dignity and worth regardless of another’s estimation of them.
Importantly, subjective ends are obtained using means that are particular to each individual’s unique contexts. For example, the means I would take to obtain a promotion within academia differ widely from the means a person working in the financial sector might undertake to obtain a promotion. Also, subjective ends are often, themselves, merely a means to a further end: I desire a new car because it will improve my morning commute, which I desire because it will improve my work performance, which I desire because it will better my chances at a promotion, and so on. Objective ends, on the other hand, are obtained by following duties that we preform irrespective of our individual contexts. To give an example from medical ethics, the surgeon performs life-saving surgery on the serial killer not because they have a desire to save a serial killer’s life but rather because they have a duty as a surgeon to preserve human life. Additionally, objective ends are what Kant calls ends in themselves – they require no further value beyond the value contained in themselves. Writing in 1785, Kant says humans can grasp inherent value through philosophical self-reflection in a way that other beings cannot – and that chief among things vested with inherent value is a human (including the experimenter himself).
Here is where Forssmann went wrong. Though it cannot be denied that he was successful in advancing scientific and medical progress, he disregarded the moral duty he had to respect himself by not treating himself merely as a means to his subjective ends. Werner Forssmann touched his own heart, shattering taboos that surrounded this vital organ and spurring a renaissance in cardiology that continues into the present day. Yet, the ethical coda to his experiment reiterates the importance of self-respect and portrays the moral limits of our scientific curiosity. This coda is timelier than ever because gene-editing technologies such as CRISPR have made medical experimentation a ‘do it yourself’-friendly endeavour. While it is unlikely that medical self-experimentation will ever cease, we can at least be hopeful that, in the headlong rush to prove a theory or advance others’ health, those who conduct such experiments watch out for their own safety and wellbeing with more care than their predecessors.