A previously healthy middle-aged man has suffered a massive stroke from a ruptured artery in his brain and fallen into a persistent, then permanent, coma.
Now imagine that before the stroke our hypothetical patient had expressed a wish to donate his organs after his death. If neurologists could determine that the patient had no chance of recovery, then would that patient really be harmed if transplant surgeons removed life-support, such as ventilators and feeding tubes, and took his organs, instead of waiting for death by natural means? Certainly, the organ recipient would gain: waiting too long before declaring a patient dead could allow the disease process to impair organ function by decreasing blood flow to them, making those organs unsuitable for transplant.
But I contend that the donor would gain too: by harvesting his organs when he can contribute most, we would have honoured his wish to save other lives. And chances are high that we would be taking nothing from him of value. This permanently comatose patient will never see, hear, feel or even perceive the world again whether we leave his organs to whither inside him or not.
Yet harvesting a patient’s organs while he is alive raises all kinds of ethical questions and triggers multiple alarms. The issue is especially complex because biomedicine, and the very definition of death and even consciousness, are all in flux.
Take our hypothetical patient, and the nature of the coma itself. A small number of patients emerge from comas after long periods of time, regaining full consciousness with many or most of their physical and mental functions intact. Far more never recover any degree of consciousness and eventually die.
And there are many states of consciousness and wellbeing between these two extremes. Patients can recover consciousness but find they are locked into paralysed bodies, unable to communicate. They might progress to a vegetative state with sleeping and waking cycles and periods of arousal but no awareness of themselves – or they might enter what doctors call a minimally conscious state, in which they have some degree of awareness but significant, often devastating, cognitive and physical impairment.
No matter where on the spectrum a patient falls, it might be impossible to predict the likelihood of death. The Israeli prime minister Ariel Sharon suffered a haemorrhagic stroke in 2006. Although he had no chance of recovering consciousness, there was no specific point at which a neurologist could say that his death was imminent. He lived in a prolonged coma until his death in 2014.
To provide a path through the thicket, experts have introduced the so-called Dead-Donor Rule (DDR), which stipulates that donors must be dead before vital organs can be taken from their bodies for transplantation. The DDR is intended to protect severely ill patients from harm by ensuring that they are not killed for the sake of their organs, regardless of whether this action could save the lives of other patients in organ failure.
But what is death? It depends. In the United States, the DDR follows from the 1981 Uniform Determination of Death Act (UDDA), which states that an individual is dead either after irreversible cessation of circulatory or respiratory functions (heart death), or after irreversible cessation of all functions of the entire brain, including the brainstem (brain death). Heart death and brain death are not the same, but they are related because when the heart stops beating so does blood flow to the brain. Similarly, when brain processes stop, so do those of the heart.
In any event, the UDDA, today law in all 50 US states, has led to acceptance of whole-brain death as the ultimate criterion for death. Canada and all continental European countries have followed suit, while the United Kingdom and India define death as the permanent cessation of brainstem function alone. Israel and Saudi Arabia, South Africa, Japan, Australia and New Zealand also have adopted a whole-brain criterion of death, despite differences in tests used to determine it.
The upshot is that while the DDR has become the bar for organ transplantation everywhere, the definition of death continues to spark debate. Some question whether mere brain death is dead enough – for is not a beating heart a sign of life, too? Others say that brain death is too much to ask; a patient with only minimal brain function should be considered dead enough to donate organs, they contend.
Would it have been ethical to harvest Ariel Sharon’s heart and kidneys, in the years between his stroke in 2006 and his death in 2014?
Technology blurs the line further. For instance, mechanical ventilation can sustain blood circulation through the body and brain when vital organs can no longer do this on their own. Thus, the heart can be kept pumping artificially for days, months or years – even if the brain is devastated and will never function again.
It prompts the question: could we harvest organs prior to death of the brain? Would it have been ethical to harvest Ariel Sharon’s heart and kidneys, in the years between his stroke in 2006 and his death in 2014? Under the DDR in place in Israel, certainly not: in comatose patients such as Sharon, the brain functions at a level too low to sustain consciousness but enough to sustain breathing and other critical functions without mechanical support. In vegetative patients, the brain allows periods of wakefulness but no awareness of one’s self or surroundings. Yet artificial hydration and nutrition through feeding tubes are required to keep these patients alive. The brain here is alive, but barely. On the other hand, the organs can still be useful if they are perfused with blood and oxygen until the moment of harvest.
In light of all this, I suggest it is time to reconsider the constraints of the DDR, time to think about harvesting organs from some living patients – those who persistently fail to maintain consciousness before the brain is technically dead.
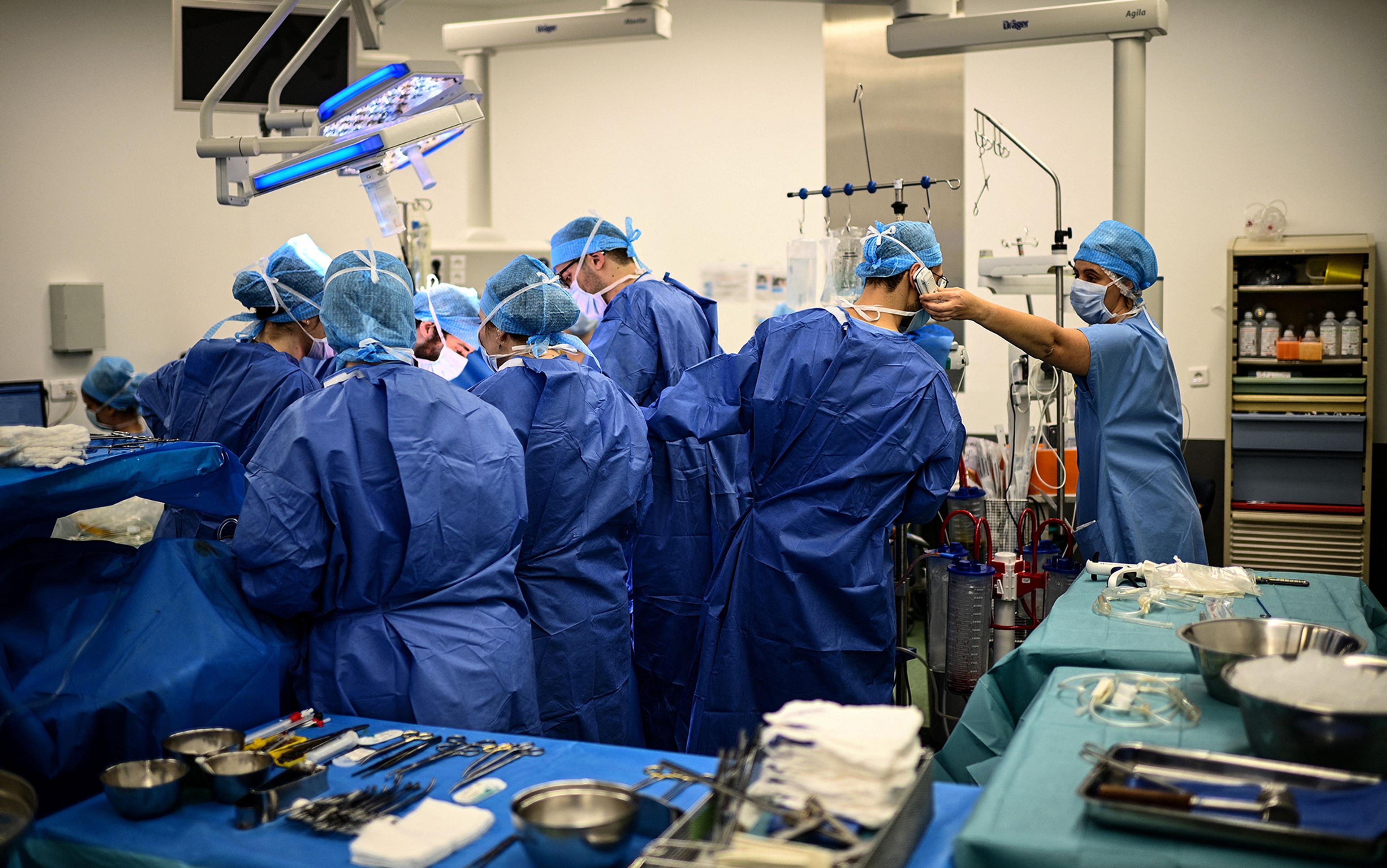
Taking organs before death already occurs on a small scale, when the procedure technically meets the requirements of the DDR. In a protocol developed by the transplant surgeon Paul Morrissey at Brown University in Rhode Island, for instance, kidneys can be taken from patients while they are alive because doing this does not cause brain death or heart death. Death is declared after the kidneys, and then life-support, are removed. This scheme applies only to kidneys, though, and is thus limited. More significantly, it reinforces the questionable claim that causing death by taking organs is always harmful to the patient and is thus morally impermissible.
But the DDR should be withdrawn in other patients, too. For instance, why apply the DDR to patients who are imminently dying? Even if conscious, such patients could be given analgesia or anaesthesia to prevent pain during organ procurement – and their organs could be put to good use.
We could also withdraw the DDR from patients who will live for years in a coma or a disordered conscious state. If a comatose patient lived for years without any capacity for consciousness, then it is difficult to understand how he would be harmed if his organs were taken from his body before a declaration of death. The same could be said about patients in a permanent vegetative state and those in a minimally conscious state with a poor prognosis.
Not so fast, you say? In some cases, a patient can emerge from a coma and regain consciousness. But this becomes less likely the longer the coma persists. And whether a patient is likely to remain in or emerge from a coma can be predicted through imaging scans showing structural and functional features of the patient’s brain. For vegetative and minimally conscious patients, the likelihood of significant improvement in physical and cognitive functions diminishes over time. The organs of those with little or no chance of improvement would better serve the body of a person who could live to the full.
In some circumstances, when donation is a high priority for an individual, we could even remove organs from those with full capacity for consciousness whose lives might go on and on in deep suffering and pain. Among the candidates include those with locked-in syndrome and amyotrophic lateral sclerosis (ALS), or Lou Gehrig’s disease, where degenerating motor neurons render the person increasingly paralysed and unable to move.
In their discussion of allowing ALS patients to donate their organs before they die, published in The Atlantic in March 2015, the transplant surgeons Joshua Mezrich and Joseph Scalea of the University of Wisconsin claimed that ‘it may be time to redefine what we really mean by harm’. It might also be time to redefine when people are harmed.
We need to get over the idea that death always harms a person and, more controversially, that taking organs before, rather than after, declaring death always harms the donor. There have been no convincing arguments for the claim that patients with no chance of meaningful recovery from progressive neurological conditions who want to donate would be harmed by organ procurement causing their death. Current legal and medical systems deny them this opportunity and are unfair to donors and recipients alike. If patients make it clear before an injury or disease onset that they would not want to continue living in such a state; if they had indicated that they wanted to be organ donors; and if anaesthesia could prevent pain, then these patients too should be candidates for harvesting alive.
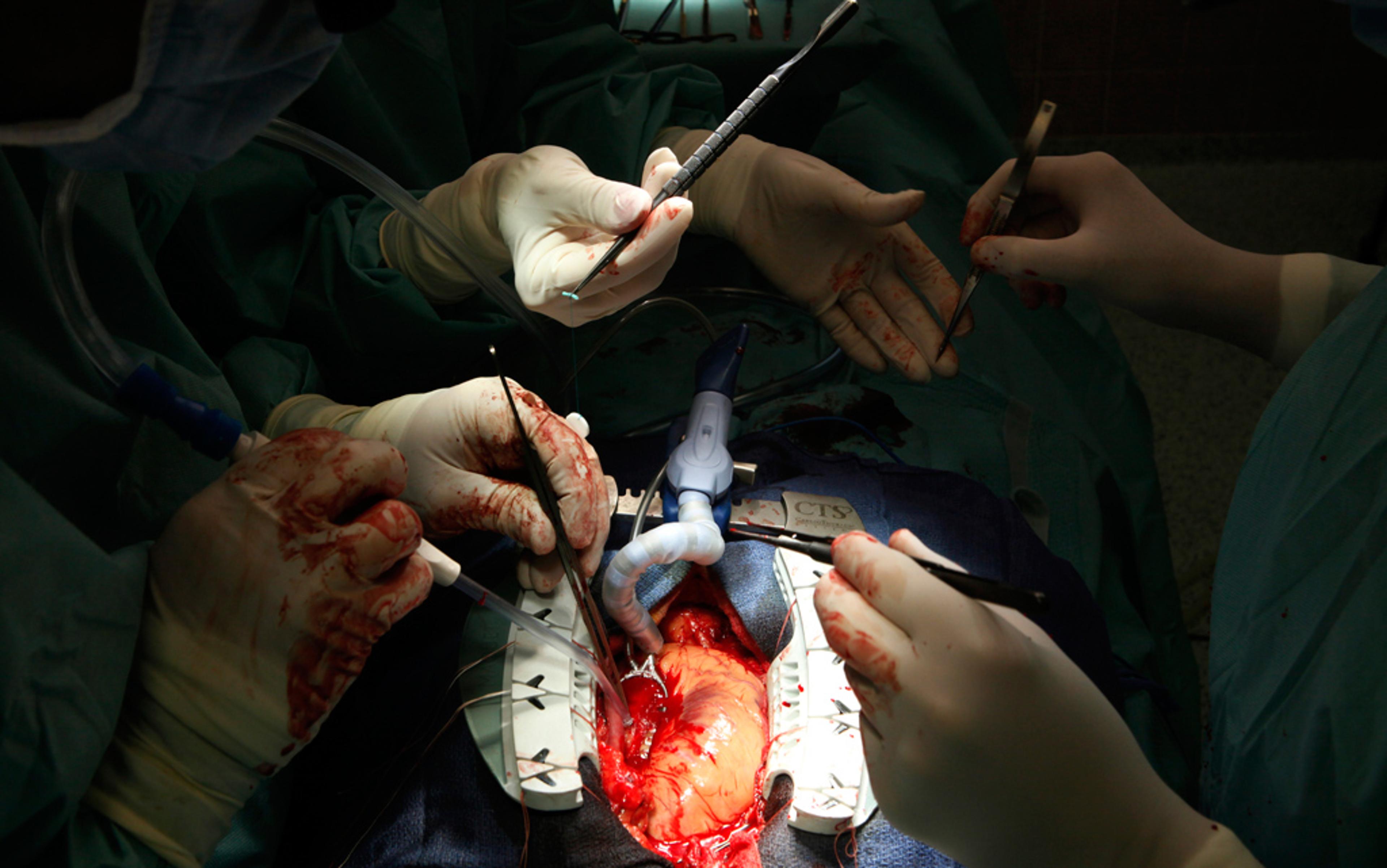
The bioethicists Dominic Wilkinson and Julian Savulescu at the University of Oxford have called transplant organ procurement before death ‘organ donation euthanasia’(ODE). ‘[W]hy should surgeons have to wait until the patient has died as a result of withdrawal of advanced life-support or even simple life-prolonging medical treatment?’ they wrote in Bioethics in 2012. ‘An alternative would be to anaesthetise the patient and remove organs, including heart and lungs. Brain death would follow removal of the heart … If there were a careful and appropriate process for selection, no patient would die who would not otherwise have died.’
‘I can’t think of a better way to undermine public support for organ transplant medicine than to permit killing for organs’
Some might ask how such a position is any different from taking organs from political prisoners or criminal offenders, as practised in China and other countries. The difference is that prisoners have not consented to organ donation. Their organs have been conscripted against their will.
In the National Review Online in 2013, the US attorney Wesley Smith, a senior fellow at the Discovery Institute in Seattle, wrote: ‘I can’t think of a better way to undermine public support for organ transplant medicine than to permit killing for organs. Not only is this kind of advocacy foolhardy, but it would have the transplant community break solemn public policy promises made to gain support from a public wary of the entire enterprise.’
He has a point. Abandoning the DDR could create public distrust in the transplant system and cause some people to opt out of organ donation for fear that they would be treated instrumentally as nothing more than a source of transplantable organs and killed for them. This could reduce the number of organs available for transplantation.
As a result, more potential transplant recipients would be harmed by poor quality of life and premature mortality from organ failure without transplantation. So there might be consequential reasons for defending the DDR and waiting until after a declaration of death before taking a patient’s organs.
Nevertheless, abandoning the DDR would remove a huge obstacle to procurement of transplantable organs. Allowing procurement before a declaration of death would redefine harm and the practice of transplantation. It would also benefit many people who need organs by saving and improving the quality of their lives.