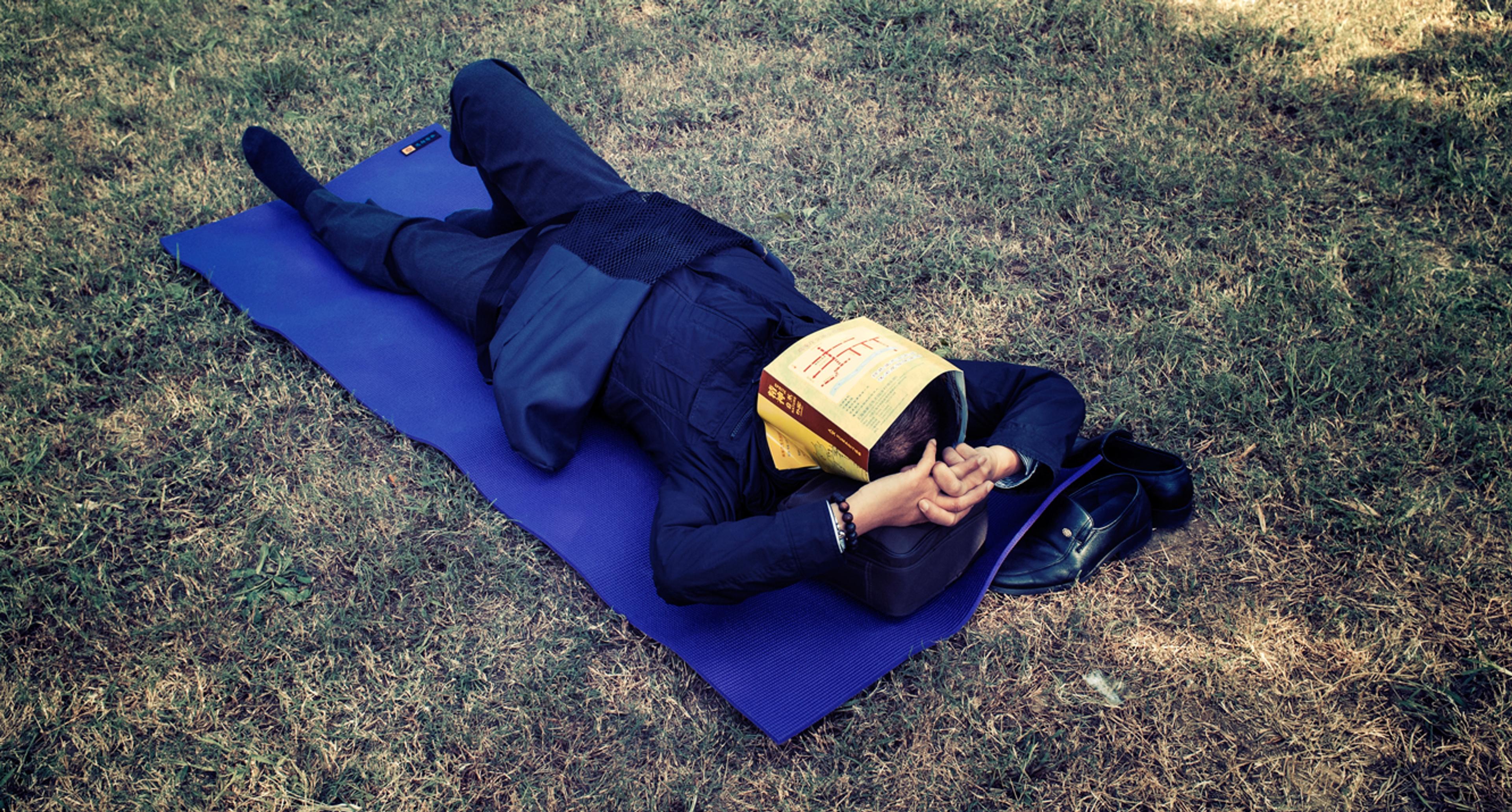
Work, friendships, exercise, parenting, eating, reading — there just aren’t enough hours in the day. To live fully, many of us carve those extra hours out of our sleep time. Then we pay for it the next day. A thirst for life leads many to pine for a drastic reduction, if not elimination, of the human need for sleep. Little wonder: if there were a widespread disease that similarly deprived people of a third of their conscious lives, the search for a cure would be lavishly funded. It’s the Holy Grail of sleep researchers, and they might be closing in.
As with most human behaviours, it’s hard to tease out our biological need for sleep from the cultural practices that interpret it. The practice of sleeping for eight hours on a soft, raised platform, alone or in pairs, is actually atypical for humans. Many traditional societies sleep more sporadically, and social activity carries on throughout the night. Group members get up when something interesting is going on, and sometimes they fall asleep in the middle of a conversation as a polite way of exiting an argument. Sleeping is universal, but there is glorious diversity in the ways we accomplish it.
Different species also seem to vary widely in their sleeping behaviours. Herbivores sleep far less than carnivores — four hours for an elephant, compared with almost 20 hours for a lion — presumably because it takes them longer to feed themselves, and vigilance is selected for. As omnivores, humans fall between the two sleep orientations. Circadian rhythms, the body’s master clock, allow us to anticipate daily environmental cycles and arrange our organ’s functions along a timeline so that they do not interfere with one another.
Our internal clock is based on a chemical oscillation, a feedback loop on the cellular level that takes 24 hours to complete and is overseen by a clump of brain cells behind our eyes (near the meeting point of our optic nerves). Even deep in a cave with no access to light or clocks, our bodies keep an internal schedule of almost exactly 24 hours. This isolated state is called ‘free-running’, and we know it’s driven from within because our body clock runs just a bit slow. When there is no light to reset it, we wake up a few minutes later each day. It’s a deeply engrained cycle found in every known multi-cellular organism, as inevitable as the rotation of the Earth — and the corresponding day-night cycles — that shaped it.
Human sleep comprises several 90-minute cycles of brain activity. In a person who is awake, electroencephalogram (EEG) readings are very complex, but as sleep sets in, the brain waves get slower, descending through Stage 1 (relaxation) and Stage 2 (light sleep) down to Stage 3 and slow-wave deep sleep. After this restorative phase, the brain has a spurt of rapid eye movement (REM) sleep, which in many ways resembles the waking brain. Woken from this phase, sleepers are likely to report dreaming.
One of the most valuable outcomes of work on sleep deprivation is the emergence of clear individual differences — groups of people who reliably perform better after sleepless nights, as well as those who suffer disproportionately. The division is quite stark and seems based on a few gene variants that code for neurotransmitter receptors, opening the possibility that it will soon be possible to tailor stimulant variety and dosage to genetic type.
Around the turn of this millennium, the biological imperative to sleep for a third of every 24-hour period began to seem quaint and unnecessary. Just as the birth control pill had uncoupled sex from reproduction, designer stimulants seemed poised to remove us yet further from the archaic requirements of the animal kingdom.
Any remedy for sleepiness must target the brain’s prefrontal cortex. The executive functions of the brain are particularly vulnerable to sleep deprivation, and people who are sleep-deprived are both more likely to take risks, and less likely to be able to make novel or imaginative decisions, or to plan a course of action. Designer stimulants such as modafinil and armodafinil (marketed as Provigil and Nuvigil) bring these areas back online and are highly effective at countering the negative effects of sleep loss. Over the course of 60 hours awake, a 400mg dose of modafinil every eight hours reinstates rested performance levels in everything from stamina for boring tasks to originality for complex ones. It staves off the risk propensity that accompanies sleepiness and brings both declarative memory (facts or personal experiences) and non-declarative memory (learned skills or unconscious associations) back up to snuff.
It’s impressive, but also roughly identical to the restorative effects of 20 mg of dextroamphetamine or 600 mg of caffeine (the equivalent of around six coffee cups). Though caffeine has a shorter half-life and has to be taken every four hours or so, it enjoys the advantages of being ubiquitous and cheap.
For any college student who has pulled an all-nighter guzzling energy drinks to finish an essay, it should come as no surprise that designer stimulants enable extended, focused work. A more challenging test, for a person wired on amphetamines, would be to successfully navigate a phone call from his or her grandmother. It is very difficult to design a stimulant that offers focus without tunnelling – that is, without losing the ability to relate well to one’s wider environment and therefore make socially nuanced decisions. Irritability and impatience grate on team dynamics and social skills, but such nuances are usually missed in drug studies, where they are usually treated as unreliable self-reported data. These problems were largely ignored in the early enthusiasm for drug-based ways to reduce sleep.
They came to light in an ingenious experimental paradigm designed at the government agency Defence Research and Development Canada. In 1996, the defence psychologist Martin Taylor paired volunteers and gave each member of the duo a map. One of the two maps had a route marked on it and the task was for the individual who had the marked map to describe it accurately enough for their partner to reproduce it on their map. Meanwhile, the researchers listened in on the verbal dialogue. Control group volunteers often introduced a landmark on the map by a question such as: ‘Do you see the park just west of the roundabout?’ Volunteers on the stimulant modafinil omitted these feedback requests, instead providing brusque, non-question instructions, such as: ‘Exit West at the roundabout, then turn left at the park.’ Their dialogues were shorter and they produced less accurate maps than control volunteers. What is more, modafinil causes an overestimation of one’s own performance: those individuals on modafinil not only performed worse, but were less likely to notice that they did.
The friendly fire incident resulted in a court martial, but in the media it was the drugs that were on trial
One reason why stimulants have proved a disappointment in reducing sleep is that we still don’t really understand enough about why we sleep in the first place. More than a hundred years of sleep deprivation studies have confirmed the truism that sleep deprivation makes people sleepy. Slow reaction times, reduced information processing capacity, and failures of sustained attention are all part of sleepiness, but the most reliable indicator is shortened sleep latency, or the tendency to fall asleep faster when lying in a dark room. An exasperatingly recursive conclusion remains that sleep’s primary function is to maintain our wakefulness during the day.
Since stimulants have failed to offer a biological substitute for sleep, the new watchword of sleep innovators is ‘efficiency’, which means in effect reducing the number of hours of sleep needed for full functionality. The Defense Advanced Research Projects Agency (DARPA) – the research arm of the US military – leads the way in squeezing a full night’s sleep into fewer hours, by forcing sleep the moment head meets pillow, and by concentrating that sleep into only the most restorative stages. Soldiers on active duty need to function at their cognitive and physiological best, even when they are getting only a few hours sleep in a 24-hour cycle.
Nancy Wesensten, a psychologist for the Center for Military Psychiatry and Neuroscience at the Walter Reed Army Institute of Research in Maryland, has a mission to find ways to sustain soldier operations for longer, fighting the effects of acute or chronic sleep deprivation. She has argued that individual’s sleep should be regarded as an important resource, just like food or fuel. Working with the Marine corps, Wesensten is not trying to create a super warrior who can stay awake indefinitely. She does not even see herself trying to enhance performance, as she already considers her subjects the elite of the elite. Everyone has to sleep eventually, but the theatre of war requires soldiers to stay awake and alert for long stretches at a time.
Whereas the US Army and Air Force have a long history of adopting stimulants — pioneering modafinil applications and dextroamphetamine use in 24-hour flights — the Marines generally will not accept any pharmacological intervention. Like Wesensten, Chris Berka, the co-founder of Advanced Brain Monitoring (ABM), one of DARPA’s research partners, told me that she is cautious about the usefulness of stimulants, ‘Every so often, a new stimulant comes along, and it works well, and there’s a lot of interest, and then you don’t hear anything more about it, because it has its limitations.’
Some failed Air Force missions have drawn attention to the dangers of amphetamine-induced paranoia. Less than a decade after a 1992 Air Force ban on amphetamines, ‘go pills’ were quietly reintroduced to combat pilots for long sorties during the war in Afghanistan. On 17 April 2002, Major Harry Schmidt, who had trained as a top gun fighter pilot, was flying an F-16 fighter jet over Kandahar. Canadian soldiers below him were conducting an exercise, and controllers told Schmidt to hold his fire. Convinced he was under attack, the speed-addled pilot let loose and killed four Canadian soldiers. The friendly fire incident resulted in a court martial, but in the media it was the drugs that were on trial.
With military personnel in mind, ABM has developed a mask called the Somneo Sleep Trainer that exploits one- or two-hour windows for strategic naps in mobile sleeping environments. Screening out ambient noise and visual distractions, the mask carries a heating element around the eyes, based on the finding that facial warming helps send people to sleep. It also carries a blue light that gradually brightens as your set alarm time approaches, suppressing the sleep hormone melatonin for a less groggy awakening.
Sleep ideally contains multiple 60- to 90-minute cycles, from slow-wave sleep back up to REM, but a 20-minute nap is all about dipping into Stage 2 as quickly as possible. The idea of the Somneo is to fast-track through Stage 1 sleep, a gateway stage with few inherent benefits, and enter Stage 2, which at least restores fatigued muscles and replenishes alertness.
For Marines at Camp Pendleton near San Diego, four hours of sleep or less is one of the rigours of both basic and advanced training. As a character-building stressor, night after night of privation is a personal endurance test but, as Wesensten has argued, it runs counter to other goals of their training, such as learning how to handle guns safely, and then remembering that information in a month’s time. Berka agrees. ‘We demonstrated cumulative effects of chronic sleep deprivation, even prior to deployment, and it was having an impact on learning and memory,’ she explained, after ABM had brought brain-monitoring devices into the camp for 28 days of measurement. ‘It was defeating the purpose of training for new skill sets, and command acknowledged this was important.’ It’s not cheap to equip dozens of trainees with night goggles and train them to distinguish foes from friends — all the while paying out salaries.
Darkness and diet are ways of practising ‘sleep hygiene’, or a suite of behaviours to optimise a healthy slumber
The Somneo mask is only one of many attempts to maintain clarity in the mind of a soldier. Another initiative involves dietary supplements. Omega-3 fatty acids, such as those found in fish oils, sustain performance over 48 hours without sleep — as well as boosting attention and learning — and Marines can expect to see more of the nutritional supplement making its way into rations. The question remains whether measures that block short-term sleep deprivation symptoms will also protect against its long-term effects. A scan of the literature warns us that years of sleep deficit will make us fat, sick and stupid. A growing list of ailments has been linked to circadian disturbance as a risk factor.
Both the Somneo mask and the supplements — in other words, darkness and diet — are ways of practising ‘sleep hygiene’, or a suite of behaviours to optimise a healthy slumber. These can bring the effect of a truncated night’s rest up to the expected norm — eight hours of satisfying shut-eye. But proponents of human enhancement aren’t satisfied with normal. Always pushing the boundaries, some techno-pioneers will go to radical lengths to shrug off the need for sleep altogether.
Charles ‘Chip’ Fisher, an entrepreneur from New York, sits in front of a full bookcase, hands folded, ready to pitch his product to the internet. On a polished dark wood table in front of him rests the device, consisting of a power source that delivers electrical current to two spongy yellow spheres. To begin the online instructional video, Fisher dips the sponges in a glass of water and tucks them, dripping, under a headband, just above his sideburns. The device is dialled up, and Fisher blinks calmly into the camera as the pulses penetrate his skull to the prefrontal cortical area of his brain. What distinguishes his device — FDA approved since 1991 — from the kind of quack products flogged to impulse-buyers is that it is staggeringly effective at treating insomnia, among other ailments. It’s also part of a new class of armament in the war against sleep.
Fisher is the president of Fisher Wallace Laboratories of Madison Avenue in New York, and the consumer electronics industry has been a family affair for him since the golden age of the vacuum tube, when his father’s company marketed the ubiquitous Fisher Radio receivers. His pitch has all the trappings of a late-night infomercial — the testimonials, the money-back guarantee, the clips from mid-tier CBS television shows — every kind of emotional argument likely to sway a rationalist away from a purchase. Fisher acquired the patent for a transcranial stimulation device from the brothers Saul and Bernard Liss, both electrical engineers from the Massachusetts Institute of Technology. He sees the body as a collection of materials, some more conductive and others more resistant to electricity. ‘The need to pierce bone and skull means we need a higher carrier frequency, which is the 15,000 Hz frequency. That’s combined with 500 Hz and 15 Hz,’ Fisher told me. ‘It took eight to 12 years to derive those values. The body is influenced by frequencies between zero and 40 Hz.’ Those searching for a treatment for insomnia are Fisher’s biggest and fastest-growing market. Someone with intractable insomnia will try just about anything to get some sleep.
Transcranial direct-current stimulation (tDCS) is a promising technology in the field of sleep efficiency and cognitive enhancement. Alternating current administered to the dorsolateral prefrontal cortex through the thinnest part of the skull has beneficial effects almost as mysterious as electroconvulsive therapy (ECT), its amnesia-inducing ancestor. Also known as ‘shock therapy’, ECT earned a bad name through overuse, epitomised in Ken Kesey’s novel One Flew Over the Cuckoo’s Nest (1962) and its 1975 film adaptation, but it is surprisingly effective in alleviating severe depression. We don’t really understand why this works, and even in today’s milder and more targeted ECT, side effects make it a last resort for cases that don’t respond to drug treatment. In contrast to ECT, tDCS uses a very mild charge, not enough directly to cause neurons to fire, but just enough to slightly change their polarisation, lowering the threshold at which they do so.
Electrodes on the scalp above the hairline, in line with the temples, deliver a slight, brief tingling, after which there is no sensation of anything amiss. ‘We use that tingling feeling to create our sham paradigm,’ Andy McKinley of the US Air Force Research Laboratory’s Human Effectiveness Directorate told me. ‘The control subjects receive only a few seconds of stimulation — not enough to have any cognitive effects but enough to give them the same sensation on their skin.’ After a half-hour session of the real treatment, subjects are energised, focused and keenly awake. They learn visual search skills at double the speed, and their subsequent sleep — as long as it does not fall directly after the stimulation session — is more consolidated, with briefer waking periods and longer deep-sleep sessions. To combat insomnia, this type of treatment is used daily in two-week sessions, according to clinical recommendations by Richard Brown, professor of psychiatry at Columbia University College of Physicians and Surgeons. The mechanism might lie in its anti-anxiety effects: patients familiar with Xanax or Valium describe their post-tCDS mood as a clear-headed version of taking these medications.
Negative effects on the brain have not yet been observed, and the FDA has approved some devices, such as the Fisher Wallace Stimulator, for unsupervised home use, but long-term effects are still unknown. The neurologist Soroush Zaghi and his team at Harvard Medical School are on the trail of how, exactly, these clinical outcomes are achieved. Once this is established, potential dangers will be easier to look for.
Using a slightly different technique — transcranial magnetic stimulation (TMS), which directly causes neurons to fire — neuroscientists at Duke University have been able to induce slow-wave oscillations, the once-per-second ripples of brain activity that we see in deep sleep. Targeting a central region at the top of the scalp, slow-frequency pulses reach the neural area where slow-wave sleep is generated, after which it propagates to the rest of the brain. Whereas the Somneo mask is designed to send its wearers into a light sleep faster, TMS devices might be able to launch us straight into deep sleep at the flip of a switch. Full control of our sleep cycles could maximise time spent in slow-wave sleep and REM, ensuring full physical and mental benefits while cutting sleep time in half. Your four hours of sleep could feel like someone else’s eight. Imagine being able to read an extra book every week — the time adds up quickly.
Never mind that if we are to speak of maintaining natural sleep patterns, that ship sailed as soon as artificial light turned every indoor environment into a perpetual mid-afternoon in May
The question is whether the strangeness of the idea will keep us from accepting it. If society rejects sleep curtailment, it won’t be a biological issue; rather, the resistance will be cultural. The war against sleep is inextricably linked with debates over human enhancement, because an eight-hour consolidated sleep is the ultimate cognitive enhancer. Sleepiness and a lack of mental focus are indistinguishable, and many of the pharmaceutically based cognitive enhancers on the market work to combat both. If only it were possible for the restorative functions that happen during sleep to occur simply during waking hours instead. One reason why we need to shut down our conscious selves to perform routine maintenance is that our visual system is so greedy. Glucose metabolism is a zero-sum game, and functional MRI studies show a radically different pattern of glucose metabolism during sleep, with distinct regions activated either in active or sleep states but not in both. As soon as we close our eyes for sleep, a large proportion of available energy is freed up. Just as most planes must be grounded to refuel, we must be asleep to restore our brains for the next day. A radical sleep technology would permit the equivalent of aerial refuelling, which extends the range of a single flight (or waking day).
Such attempts are likely to meet with powerful resistance from a culture that assumes that ‘natural’ is ‘optimal’. Perceptions of what is within normal range dictate what sort of human performance enhancement is medically acceptable, above which ethics review boards get cagey. Never mind that these bell curves have shifted radically throughout history. Never mind that if we are to speak of maintaining natural sleep patterns, that ship sailed as soon as artificial light turned every indoor environment into a perpetual mid-afternoon in May.
Our contemporary sleep habits are not in any sense natural and ancestral human sleeping patterns would be very difficult to integrate into modern life. In the 1990s, the psychiatrist Thomas Wehr of the National Institute of Mental Health in Maryland put subjects on a natural lighting schedule and observed complex sleeping rhythms. Falling asleep at dusk and waking at dawn, volunteers experienced a sort of anti-nap in the middle of the night — a two-hour period of quiet, meditative repose during which prolactin levels spiked. This is backed up by historical records from pre-industrial times: early modern English households observed ‘first sleep’ and ‘second sleep’, with the time in between used to pray or socialise with family members.
Human enhancement is now being driven by military imperatives, at least in the US, because civilian society is more conservative in its approach. Dedicated divisions such as the US Air Force’s Human Effectiveness Directorate try to make humans better at what they do naturally. It’s a missed opportunity for a society-wide push to understand and reduce our need to power the brain down for hours every day. Every hour we sleep is an hour we are not working, finding mates, or teaching our children; if sleep does not have a vital adaptive function to pay for its staggering opportunity cost, it could be ‘the greatest mistake the evolutionary process ever made’, in the words of Allan Rechtschaffen, the pioneering sleep researcher and professor of psychiatry at the University of Chicago.
In her award-winning Beggars trilogy of the 1990s, the American science fiction writer Nancy Kress posited a world in which genetic modification has become de rigeur. One of these ‘genemods’ — cooked up by gifted children let loose in a lab — eliminates sleep and even bucks the sci-fi convention of dire side effects, instead endowing the fortunate Sleepless with bonuses of greater intelligence and emotional stability. The side effects are, instead, societal — the unevenly distributed technology becomes the basis of a social schism, in which a perpetually productive elite rules a sleep-dependent majority of Livers. Kress presciently anticipated the ethical implications of our emerging era of what the neuroscientist Roy Hamilton of the University of Pennsylvania has dubbed ‘cosmetic neuroscience’, or the tailoring of our ancient brains to suit our modern demands.
Should technologies such as tDCS prove safe and become widely available, they would represent an alternate route to human longevity, extending our conscious lifespan by as much as 50 per cent. Many of us cherish the time we spend in bed, but we don’t consciously experience most of our sleeping hours — if they were reduced without extra fatigue, we might scarcely notice a difference except for all those open, new hours in our night time existence. Lifespan statistics often adjust for time spent disabled by illness, but they rarely account for the ultimate debilitation: lack of consciousness. Now a life lived at 150 per cent might be within our grasp. Are we brave enough to choose it?