In the late 1980s, aged 12, Taryn was taken to her doctor’s office with cramping, bloating, and constipation after eating, and was told that she had ‘a nervous stomach’. As a white girl growing up in New Jersey, she met a stereotype, and when initial bloodwork and imaging was negative for evidence of a ‘real’, or organic disease in her gut, one of Taryn’s doctors began writing in her charts that she had irritable bowel syndrome (IBS), a misdiagnosis that would follow Taryn for life.
At the time, IBS was considered by many to be a medically unexplained and therefore controversial illness, keeping company with conditions such as fibromyalgia and chronic fatigue syndrome. As a result, it carried the stigma of being a psychosomatic illness, caused primarily by stress and anxiety, and Taryn was sent home with prescriptions for diet and exercise. Later, when she was in middle school, Taryn was found to weigh only 80 lbs (36 kg). She was skin and bones, she told me in an interview. She couldn’t eat without throwing up or becoming ill. Blood tests revealed that she was severely malnourished, and as a consequence she was hospitalised, not to look for an organic disease, but for a presumed eating disorder like anorexia nervosa.
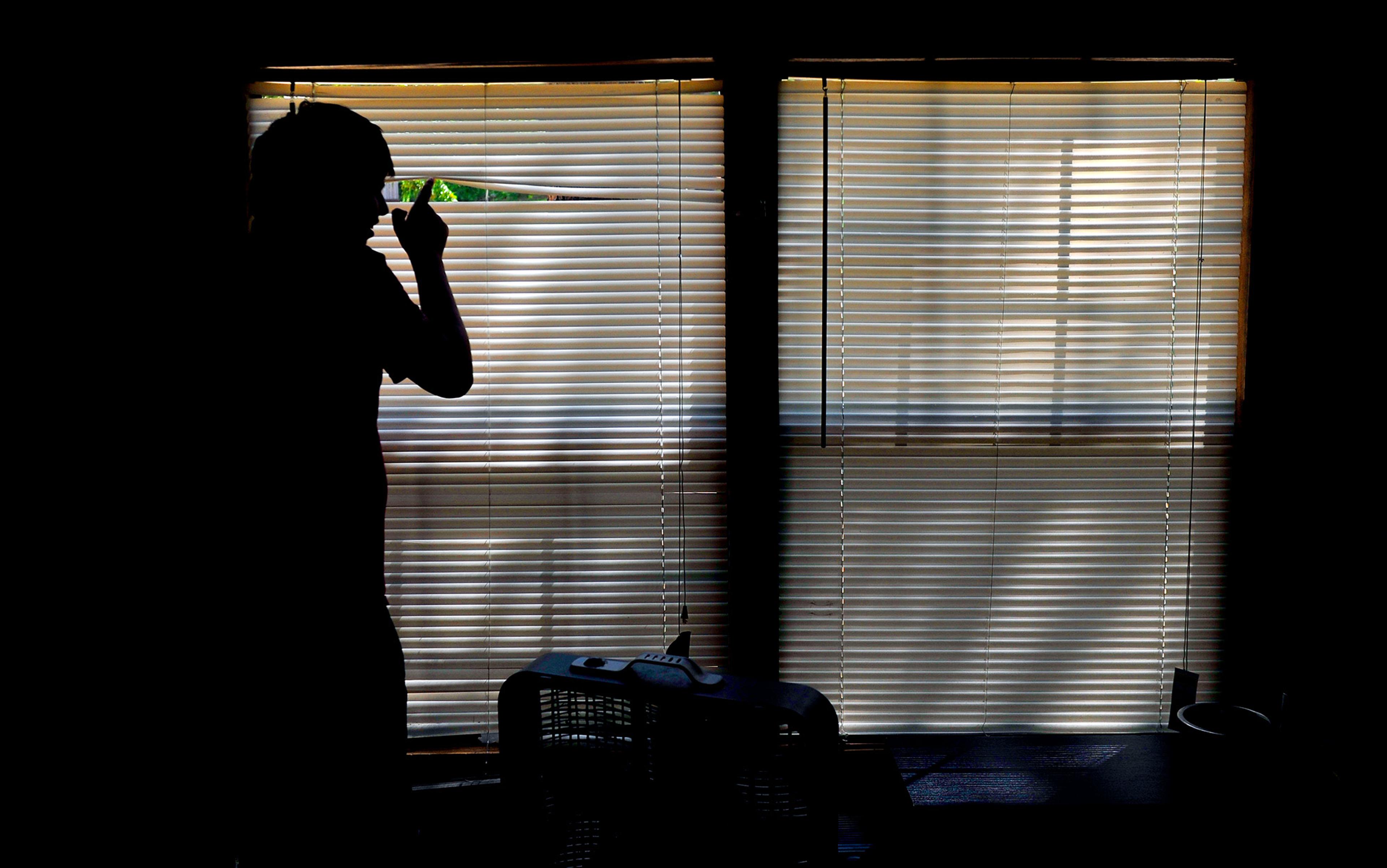
Eating disorders, much like IBS, are to this day stigmatised as forms of mental illness found in young middle-class white women, and therefore not seen as legitimate, as ‘true’ biological disease. Decades in the future, Taryn would learn from a rheumatologist that her symptoms were most likely caused by mixed connective tissue disease (MCTD), a rare autoimmune condition, not a mental illness. But, as a child, her voice had mattered very little in the paternalistic world of academic medicine. ‘Being hospitalised traumatised me,’ she said. ‘It made me distrust the medical system forever.’ Instead of being appropriately tested and treated for a gastrointestinal condition, Taryn was discharged with antidepressants and instructions to undergo psychotherapy.
Unsurprisingly, Taryn’s health continued to decline. Well into her 20s, she dealt with long episodes of extreme exhaustion and weakness, all the while trying to navigate the formative years of her youth and the long line of doctors who repeatedly said that there was nothing wrong with her. Because she couldn’t eat food, it became difficult for her to be part of social gatherings with friends and family. Her malnutrition continued to worsen to the point that her parents resorted to force-feeding, which only alienated her further, and also failed to improve her symptoms. Somehow, through all of this, Taryn managed to complete both college and nursing school, buoyed by an early childhood experience of caring for an ailing relative.
‘I was wasting away,’ Taryn told me. ‘My iron levels were so low I couldn’t walk a block without collapsing.’ For a time, she was able to ease her dependence on her parents and work as a nurse, a job she loved. One doctor, appalled that Taryn’s gastroenterologists had allowed her malnutrition to persist for so many years, placed her on a treatment called parenteral nutrition, which uses a hand-held pump to squeeze nutrient-rich fluid through a series of tubes into a catheter buried in Taryn’s chest. This bypasses the GI tract entirely and infuses minerals and nutrients directly into the bloodstream over the course of several hours. With the help of her husband, she hooks herself up before going to bed and remains there until the time when most people are eating lunch. This is still how she lives.
New obstacles arose in middle age. When Taryn’s weight, still under 100 lbs (45 kg), didn’t increase as much as expected on parenteral nutrition, her doctor accused her of sabotaging the treatment. Only later, when she found a new doctor, did she learn from an ultrasound that, while she was being kept alive on parenteral nutrition, oxygenated blood had stopped flowing to her gut, an irreversible condition called chronic mesenteric ischemia. The reason she couldn’t stomach food, the doctor realised, was that her gut didn’t have enough blood supply to effectively absorb anything she tried to eat. The diagnosis had never been IBS, or an eating disorder at all, but an underlying autoimmune process that caused long-lasting inflammation of her blood vessels. And now, because of these misdiagnoses and flat-out medical gaslighting, the true source of Taryn’s suffering had been left to develop unchecked, and had permanently disabled her ability to eat. The only solution was to undergo an intestinal transplant. Finally, she thought, she had proof that her illness was ‘real’.
Today, unlike in the 1990s, it is well established that conditions like IBS, collectively known as disorders of gut-brain interaction (DGBIs), are real diseases that disrupt the communication between the nervous system of the brain and spine, and the nervous system of the intestines. First mentioned in the book The Irritable Gut (1979) by the gastroenterologist W Grant Thompson, the conditions were labelled ‘functional’ disorders – characterised not by structural damage to the hardware of the gut, but by a glitch in its ‘software’, in other words, its nervous system, charged with processing, receiving or relaying information coming in or going out. Software is not as easily observed as hardware, however, and much of academic medicine views the mind and the body as two separate and distinct entities, a viewpoint called mind-body dualism. Over time, and despite the more nuanced meaning intended by Thompson, the term ‘functional’ became associated exclusively with disorders of the mind.
This is part of the reason why there is still stigma against conditions like IBS, and why attempts to establish diagnostic criteria for IBS in particular suffered from vagueness. For centuries, there had been little agreement about how to even name the mysterious illness, and IBS went by names like mucous colitis, membranous enteritis, tubular diarrhoea, mucous colic, and myxoneurosis intestinalis. It was not until 2016 with the fourth iteration of what are called the Rome Criteria – a set of guidelines for IBS and other, similar diagnoses – that there has been a precise enough definition to dispel the label of functional disorders for good.
In the US, managing IBS makes up about 12 per cent of primary care visits
To meet the criteria for IBS today, a patient must have abdominal pain at least once a week for three months, which must be related to two or more of the following: bowel movements, changes in bowel-movement frequency, or changes in the stool appearance. There are even subtypes of IBS, which are separated by whether a patient is mostly constipated, has diarrhoea, an equal mixture of both, or a pattern consistent with neither, a condition that’s ominously called ‘IBS unclassified’.
Under these criteria, IBS has been estimated to affect roughly 4 per cent of the global adult population. The International Foundation for Gastrointestinal Disorders estimated that, in the United States alone, up to 45 million people have it, with two-thirds being women and most people affected being under the age of 50. In the US, managing IBS makes up about 12 per cent of primary care visits and is responsible for more than 2.2 million prescriptions every year, costing the medical system more than $30 billion in annual healthcare expenditures. Given how common it is and how costly its effects have been for the healthcare system, it was surprising to me how little was known about IBS up until the past few decades.
The cardinal symptoms of IBS – pain, irregular bowel movements, and bloating – have been cited as early as 400 BCE in the works of Hippocrates, the father of clinical medicine. In 1817, the English doctor William Powell was the first to link this triad of symptoms in one patient to subjective ‘feelings of oppression’. Even back then, there was a suspicion that stress and GI disfunction could be physiologically connected, rather than imagined by a patient, but more work would be needed to make that connection stick.
For much of European and US history, the various types of neuroses like hysteria and hypochondria were written about by physicians as having an organic basis, arising in various organs from the uterus to the spleen. In 1869, the US neurologist George Beard coined the term ‘neurasthenia’ to describe excessive bodily sensitivity to the environment from which neuroses could arise. But even Beard connects these subjective reactions to physical exhaustion of the brain and stomach, which suggests an organic cause at the nexus of neurology, psychiatry and modernity.
How then did IBS develop a reputation for being solely a product of mental illness? William Osler, who is considered a seminal figure in developing the field of internal medicine and an advocate for humanism in healthcare, was one of the first physicians to describe IBS in a textbook for other physicians in 1892. In it, Osler attributed the condition not only to neuroses and stress, but also to personality defects. ‘The patients are self-centred,’ he wrote. ‘Some cases have had hysterical outbreaks, and there may be hypochondriasis or melancholia … Some of the cases are among the most distressing with which we have to deal … neurasthenic to an extreme degree.’
Why such dismissal? Thompson, author of The Irritable Gut, has proposed several explanations. In his paper ‘The Road to Rome’ (2006), he explains that, in the early 20th century, disorders like IBS were seen as ‘conditions of the wealthy’ who could afford to see ‘Harley Street doctors who published their observations in the medical literature’. Proctalgia fugax, a pain syndrome of the anus that is now one of the DGBIs, was ‘long thought to be a disease of young professional males, because only doctors had the temerity to describe their symptoms in letters to the editor of The Lancet.’ As a field, Thompson observed in the paper, gastroenterology was still plagued by discredited theories – for instance, the debunked idea that toxins in retained stool could cause disease. Clinging to that disproven belief, many physicians were still encouraging their patients to undergo full purges of their intestines and even, in the case of the surgeon Sir W Arbuthnot Lane, completely removing their colons.
In utero, the precursor cells for our gut and our brain actually share the same nervous system
Language, of course, plays a major part in creating stigma about certain illnesses. In addition to pejorative words like ‘psychogenic’ and the phrase ‘the abdominal woman’ that Robert Hutchison used in his lectures on dyspepsia, there was also the introduction of the word ‘irritable’ to describe the colons of IBS patients. Irritable in a medical sense simply means that an organ is abnormally sensitive, but when applied to groups of people it suggests a mood or disposition to become angry. Writing in the Rocky Mountain Medical Journal in 1950, the physician Philip Walling Brown introduced the condition this way:
A physician is both chilled and challenged when a patient starts the conversation with the comment: ‘Doctor, I do hope you can do something for my colitis. I have been to many doctors and none of them has been able to help me.’ These remarks usually are offered by a woman but may be made by a man and, parenthetically, one might add that he is often the more difficult to satisfy.
These linguistic biases also seep into how doctors interpret research. When academics read that IBS patients have higher rates of anxiety and depression, or that antidepressants are a treatment for IBS, many assume that this is because psychiatric symptoms cause symptoms of IBS without considering the inverse, that chronic undiagnosed abdominal pain predisposes patients to having mood disorders.
The real reason these drugs are effective, however, is that, in utero, the precursor cells for our gut and our brain actually share the same nervous system, and only later separate in embryonic development. As a result, the two nervous systems utilise the same neurotransmitters, such as serotonin, to send messages between neurons. This is why we sometimes feel butterflies in our stomach when we’re nervous, and why stress and anxiety often worsen symptoms of IBS, but do not necessarily cause it.
As Brown’s quote above implies, the stereotype of the anxious patient in pain applies not only to IBS but all patients who present to clinics with vague abdominal distress (including those with non-gastrointestinal conditions like endometriosis, who experience delayed diagnosis because providers take women’s pain less seriously than men’s). A classic example is peptic ulcer disease, a cause of severe abdominal pain that for decades was denounced as a psychosomatic illness until Barry Marshall and Robin Warren discovered in 1983 that it was caused by a species of bacteria. Before their findings, peptic ulcers were managed with diet and, frequently, surgery, when what patients needed were antibiotics.
It would take 16 years for another conceptual revolution to sweep through the field with the advent of neurogastroenterology: a new lens for seeing the gut through its own nervous system, a network sensitive to a range of factors beyond the mere mechanical movement of food and nutrients through a series of channels and vents. Research now validates IBS as a software problem rooted in neurology, sometimes provoked by imbalances in the gut microbiome or acute infections such as food poisoning, other times caused by a long list of factors from alternations in the intestine’s ability to move stool, to inflammation from abnormal immune response. Why then, in the face of all this evidence and significant strides made in formalising the diagnosis of DGBIs, has the bias against patients with abdominal pain and those with IBS in particular continued to be passed down from one generation of doctors to the next?
In my opinion, the root of the problem is medical education itself. Unless a medical trainee becomes a gastroenterologist, it is unlikely that they will receive any specialised education in IBS, let alone the history of IBS research proving it to be an organic condition, despite 40 per cent of the general population having functional gastrointestinal disorders. Partly, this is because a majority of medical education in countries including the US, the UK and Canada takes place in academic centres associated with hospitals, where medical students will probably never encounter a patient for whom their IBS symptoms are the primary reason for them appearing in the emergency room, and especially not for their admission to the hospital itself.
Most of the global disease burden across the world is caused by chronic, not acute, illness
As a consequence, medical students also don’t get their knowledge of IBS tested by board examinations. This speaks to the fact that, echoing Osler, IBS generally doesn’t kill patients, and our current healthcare system values measures of mortality and cure in response to acute complaints more than quality of life and the management of suffering from chronic issues such as IBS.
The same could be said about long COVID (which, to this day, is sometimes challenged as illegitimate) and chronic fatigue syndrome, where sufferers are often sent off to a psychiatrist for care. The thinking is that these ongoing problems, where there is no mainstream route for testing and treatment, are not as important for medical students to know about compared with, say, a patient crashing after a cardiac arrest, even though most of the global disease burden across the developed and the developing world is caused by chronic, not acute, illness.
I first met Taryn in the spring of 2022 while reporting for an article on the experiences of patients who depended on home parenteral nutrition to live. At the time, I was taking a leave of absence after my third year of medical school at the University of Rochester in New York to pursue a graduate degree in creative writing. Finally, away from the whirlwind of clinical duties and examinations required in medical training, and with more time to commit to introspection of my inner world, I became increasingly aware of the field of signs and symptoms in my own body that I had ignored for years.
Filled with new medical knowledge without extensive clinical experiences, medical students get a bad rap for being prone to self-diagnosis or hypochondria. We are constantly reading our bodies for symptoms of disease that are reflected in textbooks or in our patients. As a result, I have received my fair share of eye rolls for even thinking about making an appointment with my primary care physicians to get anything more than a routine physical.
After hearing Taryn’s story, however, about how her glib misdiagnosis of IBS delayed the care she needed by many decades, I decided to look at my body for the first time with a degree of seriousness. The facts were that, starting in college, I had for years suffered from debilitating GI issues that had sometimes even impaired my ability to attend classes, out of fear of having an accident on my commute. And yet, I had never thought to see a doctor about it. Even after I learned what IBS was in school, how it was diagnosed and how it was treated – all bundled into a single one-hour lecture – I did what Taryn’s doctors did to her and stamped myself as a typical IBS patient.
I wanted to invalidate my own suffering and wish away my body from the healthcare system, lest it become an unnecessary burden to others. Even if I did see a professional, I thought, and received a diagnosis of IBS, wouldn’t they look down on me? In our only lecture on IBS, we were given a rudimentary list of treatment modalities (antidepressants, psychotherapy, yoga, fibre supplements) that made many of us, and I’m sure many of our future patients, sigh deeply. Didn’t most of us students, famous for enduring the decades-long training required to become a doctor, suffer from IBS? (In fact, one study in Karachi, Pakistan found a prevalence of 41 per cent in their medical students.) I was already taking antidepressants and undergoing psychotherapy for mental health problems. Wouldn’t doctors rightly assume that my symptoms were caused by stress?
The medical culture uses diagnoses like IBS to shuttle away patients rather than assist them in finding an answer
I told myself every excuse in the book for why my own suffering was illegitimate and, by that, I mean not unusual: I drank too much coffee, I was stressed out about school, I was a racial minority in the US, I lived under late-stage capitalism. Whatever structural forces in my life felt overwhelming and immutable I allowed to stand between me and getting care. I subconsciously absorbed and internalised all the assumptions about IBS that Osler wrote about in his guidelines on mucous colitis. I believed that my issues were not urgent, that they were the product of fixed environmental factors, and, taking into account Beard’s account of neurasthenia, that my symptoms were simply a rite of passage into the club of normal adulthood in the modern US.
But then I heard Taryn’s story, and how much time it took for specialists to diagnose MCTD and treat it with the gravity it deserved. As someone who would be responsible, one day, for treating patients fairly, and as a writer who sought to legitimise the experiences of the patients I met outside the hospital, didn’t I deserve to know the truth, and not merely an assumption, about my own body?
The current medical culture produces doctors like Taryn’s who saw that she fit a particular stereotype and acted based on bad reasoning rather than a careful consideration of diagnostic criteria. And it uses diagnoses like IBS to shuttle away patients rather than to assist them in finding an answer. Of course, an argument can be made that, when faced with vague abdominal pain without clear initial test findings, it makes sense that providers first reach for the most common diagnoses before getting more in-depth testing or a referral to a gastroenterologist.
‘It’s useful to know what’s common,’ Nitin Ahuja, a neurogastroenterologist at Penn Medicine in Philadelphia told me in an interview. ‘The imperative is for more nuance and not reaching for the most obvious heuristic. But the counterargument to that is, from a cost perspective, if you have a person who meets a pattern, you don’t want to spend a bunch of money doing unnecessary tests like multiple endoscopies. These diagnostic tests also have harms associated with them.’
This presents the inverse of Taryn’s story, where patients who do have IBS are subjected to and charged for excessive scrutiny. Cases of IBS patients undergoing unnecessary procedures, and even surgeries, are unfortunately common. One systematic review found that there is a three-fold higher risk of having a gallbladder removed and a two-fold higher risk of having an appendix or uterus removed in IBS patients. (Unsurprisingly, the specimens resected are generally normal and patients don’t experience improvements in their symptoms after surgery.)
I experienced a taste of this in my own journey to understand my IBS diagnosis. For, unlike Taryn who was told she had IBS and was then turned away, when I went to see my primary care physician for the first time, I was told I probably had IBS, but should be evaluated by a gastroenterologist just in case. Age, gender roles, the heightened fear of litigious patients and increased specialisation in the current medical field all played a part in how differently Taryn and I were treated for our GI symptoms. This reveals the dual complexity of IBS care: on the one hand, it’s a label that often allows other more debilitating diseases to go unexamined; and on the other, it’s a label that can be used to justify too much testing.
Did I, a 25-year-old with eight years of chronic GI symptoms, without red flags for colon cancer such as weight loss or a family history, really need a colonoscopy? How desperately did I want to prove that my illness had an organic basis? In the medical journal Gut, the gastroenterologist George Longstreth characterises the ‘cycle of intense, misdirected medical activity’, or furor medicus, that contributes ‘to the brain-gut dysregulation that underlies the pathophysiology of IBS and other functional gastrointestinal disorders.’ First, he discusses how patients’ frequent visits to doctors for chronic pain and disability can drain providers, who may lack knowledge of IBS (one study found that fewer than 30 per cent of non-gastroenterologists could correctly apply the Rome Criteria), surgeons in particular, by depriving them the gratification of diagnosing and curing the disease.
The desperate focus on finding an easily observable structural cause, which IBS lacks despite being an organic disease, then leads to excessive referrals, tests, treatments and surgeries. The high cost, poor outcomes and possible harms to the body from unnecessary treatments and tests then lead to dissatisfaction and a loss of control on the side of the patient, which only worsens the pain and hypervigilance that brings them to the clinic in the first place.
Diagnoses are fluid entities, labels that should be revised with every new visit
In my case, the flurry of testing brought back only one positive diagnosis. I had completed a breath test that had detected an abnormally high amount of bacteria in my intestines, a condition called small intestinal bacterial overgrowth (SIBO). Finally, after all my troubles, I had a positive diagnosis and an organic explanation for my symptoms. But I was wary of the high false-positive rates of breath tests like the one I did, which can be as high as 48 per cent, and was not surprised when two different antibiotics had no effect on me. My gastroenterologist suggested that I start an antidepressant, for the purposes of symptom management.
Oftentimes in medicine, positive diagnoses are used as mechanisms for getting patients in the door, to get insurance coverage for basic lab work and to start treatment, with the idea that, if the original diagnosis is wrong, then the patient will get worse, and we as providers can adjust accordingly. Diagnoses, then, are fluid entities, labels that should be revised with every new visit so that the patient has a stepwise progression through the view of their illness and the journey of care.
But this ideal depends on an assumption that the provider in question has the patience to look a patient in the eye and say that they don’t know what’s going on, and for the patient to follow a provider’s advice over a long stretch of time even when they’re doing worse. What would happen if IBS itself was used as a positive diagnosis, rather than as a diagnosis of exclusion, a leftover label given after exhaustive testing comes out negative, or as a careless misdiagnosis, as in Taryn’s case? What we get instead is either a blind eye or its counterpart, furor medicus.
Listening is key to building a differential diagnosis. An article for the ‘Diagnosis’ rubric of the New York Times Magazine in 2022 told of a patient who, for 24 years, was repeatedly told by countless providers in different specialties that she had IBS, while still undergoing endless testing and several trials of antiparasitic and antibiotic medications for bloating and a mixed picture of diarrhoea and constipation. It was only when a family medicine doctor spent a long time listening attentively to her history of ‘IBS’ that someone realised that her array of other symptoms (night sweats, fatigue, brain fog, musculoskeletal pain) just didn’t fit in the silo of the Rome Criteria. She was found to have a probable infection with Brucella bacterial species, and was started on the appropriate antibiotics, curing her symptoms.
There are several ‘organic’ conditions that can either lead to IBS, or mimic IBS, and if some of these other illnesses are missed by a careless provider, even if appropriate testing is conducted when the patient worsens, it could spell a devastating conclusion for that patient’s clinical course, as in Taryn’s case.
Starting with GI disorders that have symptoms typical for IBS that are imminently treatable, there have been studies that have found startlingly high rates of bacterial overgrowth in the gut (49 per cent of IBS patients), problems with absorbing sugars like lactulose and fructose (54 per cent) and defects in the gut’s ability to recycle bile (41 per cent). Obviously, it’s not possible to say whether these patients have IBS independently of these other conditions, but the fact that these entities were left undiagnosed leaves a high suspicion that the diagnosis of IBS was blocking these treatable conditions from view of their providers.
We should view the diagnoses not as separate buckets but as being on a spectrum of pain presentation
In conditions such as coeliac disease, there are clear excesses of IBS diagnoses and delays in treatment because of these misdiagnoses. A 2013 study from the UK found that 16 per cent of their coeliac patients had a prior diagnosis of IBS, compared with 5 per cent of their control patients. Another UK study from 2011 reported that early symptoms of IBS could delay diagnosis of early Crohn’s disease, and a study from 2014 found that 10 per cent of those with inflammatory bowel disease were misdiagnosed with IBS, 3 per cent for five years or more.
Part of the issue is that the diagnostic criteria of many DGBIs bleed into each other. For instance, the requirements for a patient to be diagnosed with chronic constipation are similar to the requirements for the constipation type of IBS. Many of these chronic causes of abdominal pain can also be easily mistaken for more acute causes, like diverticulitis, a common type of infection in the intestines. As Ahuja put it to me, we should view the diagnoses not as separate buckets but as being on a spectrum of pain presentation. DGBI is a broad umbrella where several diseases exist, many of which can be active simultaneously in a single patient.
Furthermore, DGBIs have an unstable temporal progression, which means that a person with one may go in and out of their condition throughout their life, whereas a diagnosis like Crohn’s disease is one you always carry with you: you either have it or you don’t. Usually, academic medicine prefers these kinds of discrete categories of disease presentation. ‘It reflects the nature of the differential diagnosis,’ Ahuja said, ‘where illnesses are like items in a checklist rather than clouds that drift into each other.’
One could certainly argue that, although IBS wasn’t the correct diagnosis for Taryn, it allowed her to receive continued evaluation and support from physicians, which did ultimately push them to the correct provider and treatment. In the future, IBS and DGBIs are increasingly being seen less as distinct disease entities and more like symptom clusters, umbrellas under which many disease entities fall. In this context, the label of IBS will hopefully serve as a foot in the door for patients to reach a trained neurogastroenterologist, arriving at a better state of health.
That world is still a long way off. Instead, the current reality is that IBS ‘diagnoses’ are still used to shut down conversations about testing for other health problems, as in Taryn’s case. In one survey study of close to 2,000 people with a history of GI symptoms, about 57 per cent met criteria for IBS but, even so, about 43 per cent had never received a medical diagnosis. Compared with undiagnosed individuals, diagnosed patients in the study were more likely to be white (93 per cent, versus 86 per cent), female (78 per cent, versus 64 per cent), and over the age of 60 (22 per cent, versus 12 per cent). These demographic patterns don’t explain who really has the disease – they just reveal medical and social bias and entrenched stereotypes: women are perceived as hysterical and diagnosis-seeking, while men are stoic and avoidant, for instance; or white women are thought to tolerate less pain than people of colour. None of this, in reality, is true – but it is part of the reason why so many patients assume that what they suffer from won’t be justified by the presence of organic disease and therefore doesn’t warrant a doctor’s visit in the first place.
Such patients, treated so poorly within the medical mainstream, now have a community and identity of their own in the Wild West of alternative medicine that flourishes online. Such groups, seeking to empower themselves and especially hoping to get well, today stand at loggerheads with the practices and physicians they have left behind.
Some accuse their former doctors of gaslighting them, and they deserve to be heard. Much of what I have discussed regarding misdiagnoses of IBS assumes that healthcare providers, even when in error, always have good intentions and are sincere about using the diagnosis to clarify the patient’s medical case. There were several elements of Taryn’s story, however, and in my own experiences of how DGBIs are taught in medical school, that make it difficult for me to believe that this assumption holds in most doctor visits. Although one could argue that the blasé diagnoses of IBS and disordered eating for Taryn could be down to simple carelessness and negligence, honest errors, or someone being ‘just a bad doctor’, it’s obvious to me that a pattern was developing with Taryn’s interactions with different providers who weren’t taking her lived experience itself seriously, just as I had stopped taking my own experiences seriously.
The physician doubted her sincerity and competence, and imposed his own narrative on her experience
What holds our stories together, I believe, is this phenomenon where both of our perceptions of our own ability to know what’s true or not were put into question. In her 2023 essay in The Philosophical Quarterly, Elizabeth Barnes points out that this sensation is the basis for the term ‘gaslighting’, at baseline a reference ‘to situations in which a person is made to doubt aspects of their own experience over which they would ordinarily be considered an authority, and ordinarily have no reason to question.’ Medical gaslighting is a common experience for chronically ill patients who feel they’ve lost control over their body, not only from illness but also thanks to the providers who have power over them. ‘Medical gaslighting,’ Barnes writes, ‘refers to situations in which physicians dismiss a patient’s account of their own symptoms as unserious, perfectly normal, perhaps psychosomatic manifestations of stress, etc.’ Women, people of colour and patients with controversial/contested illnesses like long COVID, chronic fatigue syndrome and IBS are especially vulnerable because they are disproportionately prone to being disbelieved and have the ‘physiological seriousness’ of their conditions minimised.
Would Taryn’s example of receiving a flippant IBS diagnosis count as an example of gaslighting, or would it be an example of a missed diagnosis or a provider being a bad doctor? ‘[I]n some instances,’ Barnes writes, ‘the stories involved seem to be simple instances of misdiagnosis – something that can be incredibly frustrating, destabilising, and harmful, but that isn’t always blameworthy, and is an inevitable reality of medicine. Sometimes, even the most conscientious doctors will get things wrong. Mistakes in diagnosis will cause harm (especially to patients), but they don’t necessarily represent blameworthy lapses.’
The devastating aspect of Taryn’s story, however, is that these seemingly non-blameworthy lapses had real consequences for her future care, and may have predisposed a physician to disbelieve that she was taking her home parenteral nutrition appropriately, a traumatising experience. This situation much more resembles the original definition of gaslighting, in which a person ‘is made to doubt aspects of their own experience over which they would ordinarily be considered an authority, and ordinarily have no reason to question.’ In other words, because the physician doubted both Taryn’s sincerity and her competence as a patient, he imposed his own narrative on her experience, thereby undermining her authority over her own story.
This is no longer a case of mere incompetence or scepticism, I would argue, but a hermeneutic of distrust that’s based in a fundamental disbelief in the patient’s self-authority, which then infects the patient and those around her. Part of this could certainly be chalked up to the personalities of individual physicians, but I believe that there are also structural effects of stigma against diagnoses like IBS and disordered eating, wrongly seen as controversial, which scar a patient’s medical record and encourage this harmful sort of doubt about the aetiology of suffering.
Taryn’s entire medical history functions, for me, as both a parallel and an extreme allegory for how misdiagnoses of DGBIs can jeopardise a patient’s long-term health. I use the word allegory intentionally, because my having the opportunity to listen to and analyse her story was the initial impetus for me to question my own biases against IBS and my internalised sense of distrust about my own ability to know my body, which eventually led me to seek testing and care for my underlying medical condition.
This is the alternative route to our current social media hivemind around digestive suffering. While the mass homogenisation of online illness communities can create complacency and a sense that one’s symptoms are ‘normal’, the one-on-one encounter with another’s illness story can often be more effective at conveying information about medicine than consultations with potentially biased providers. Moreover, patient voices have a clear role to play in the education of healthcare professionals themselves, not only in providing additional details about illness (expecting more physicians to learn the Rome Criteria is, I would argue, an insufficient solution), but also in creating an institutional atmosphere of patient-centred care and trust.
Who, in the patient-physician relationship, is allowed to play the roles of teacher and storyteller?
As authors in The BMJ Opinion column wrote in 2019:
By its very nature, the active inclusion of patient narratives disrupts traditional power hierarchies that have permeated healthcare education and regulation for decades. By respecting patient narratives as an equal source of knowledge and evidence, the passive ‘outsider’, a role traditionally held by patients, becomes an active educator to the elite ‘insider’, but only if permitted…
A model of mutual trust therefore requires a radical shifting of our conceptions of who, in the patient-physician relationship, is allowed to play the roles of teacher and storyteller.
In a world driven by data, it is important to remember that narratives are a form of evidence. They are not ‘soft’. They are a constructed version of reality, a permanent reminder of an encounter that left a lasting impression. It’s vitally important that they are treated with the value and respect that they deserve.
Paradoxically, this aligns with the model of mutual distrust that Barnes advocates for at the conclusion of her essay, in which neither doctor nor patient fully defers authority over the illness narrative to the other. Providers acknowledge the patient’s understanding of their suffering but not necessarily the patient’s statements about the aetiology of their suffering, and patients recognise the provider’s expertise in light of the fact that many are either not well trained or are biased in regard to DGBIs. In this model, the doctor needs to earn the patient’s trust by first being open and soliciting the patient’s first-person narrative of their experiences, while also giving the patient room to advocate for themselves, seek second opinions, and revise their own beliefs at the intersection of medical advice and other patients’ stories. Only then can the diagnosis of ‘just IBS’ become the beginning, rather than the coda, of the beautifully varied relationships shared between patients and providers.