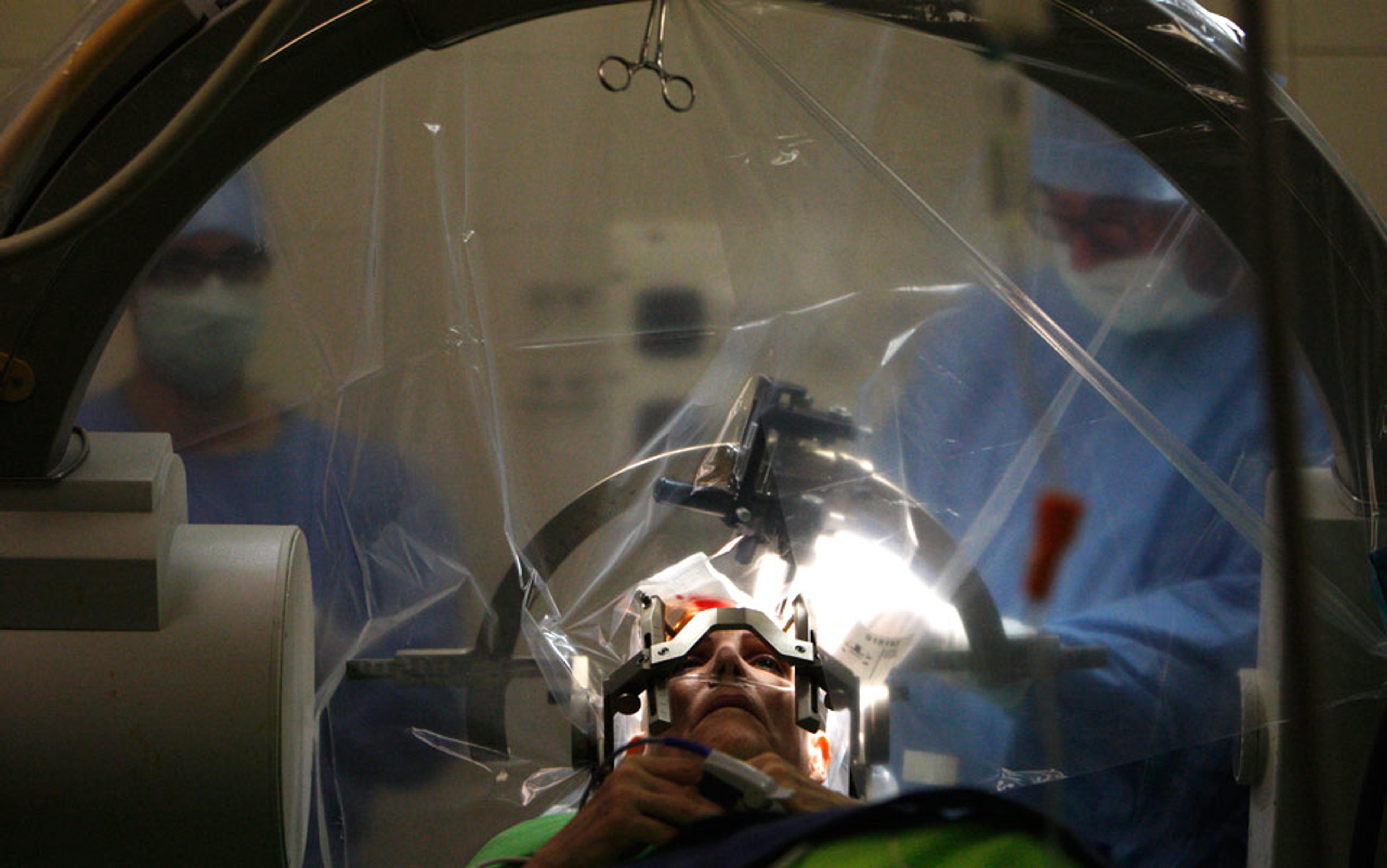
Picture yourself in a lab, expecting to start a new kind of clinical treatment for anxiety. You’re nervous, your mind filled with thoughts of syringes and little white pills. Sterile walls line the hallways as you tiptoe into a room marked ‘Neurology’. But when you enter, all you see is a huge, donut-shaped tube. A discreet, white-coated attendant enters and asks you to lie down on an extended bed or ‘boor’ (as he calls it), telling you that he’s just going to wheel you into a scanner. Try to adopt a state of mind that makes the picture you’ll see get bigger, he says. That’s all.
As you lie quietly inside the machine and start to relax, an image appears on a screen in front of you: a small black circle that gets wider and wider every few seconds. As you continue to unwind, the circle grows a little bit bigger, and bigger again. At the same time, you can feel your anxiety ebbing slightly. You hear a sound from outside your field of vision, perhaps another researcher scuttling into the room; you lose focus for a moment, and notice when your gaze returns to the screen that the circle has diminished to barely a pinprick. You try to relax again, and see that the circle expands more quickly this time. You seem to be getting the hang of it. A smile breaks across your face. This seems pretty easy, you think; with a sigh of relief, the circle grows just a little bit more.
This technique is known as neurofeedback. It’s one of the most promising and rapidly advancing frontiers in mental health. By linking brain activity to an image or sound in real time, we can use simple game-like techniques to get people to train themselves to forge new neural connections and voluntarily adopt (or avoid) certain mental states. Like a thermometer going up and down according to temperature, the fact that people can see and hear what their brain is doing provides a lever that allows them to internally regulate their own mind, without the need to engage in more direct behavioural interventions.
Neurofeedback represents a big leap for many clinical mental disorders such as phobias, anxiety and post-traumatic stress disorder (PTSD) – all of which can be difficult to address because the experience of them can be so overwhelming. For these illnesses, cognitive behavioural therapy (CBT) is a standard treatment. It requires individuals to face up to their fears; typically, patients will undergo multiple sessions in which they are exposed to ‘triggers’, so that they eventually learn that the triggers don’t pose an objective threat. If you’re terrified of spiders, for example, you might be forced to sit in a room with a spider to try to overcome your fear. But this is such an unappealing prospect that many people end treatments early, and interventions have a low success rate.
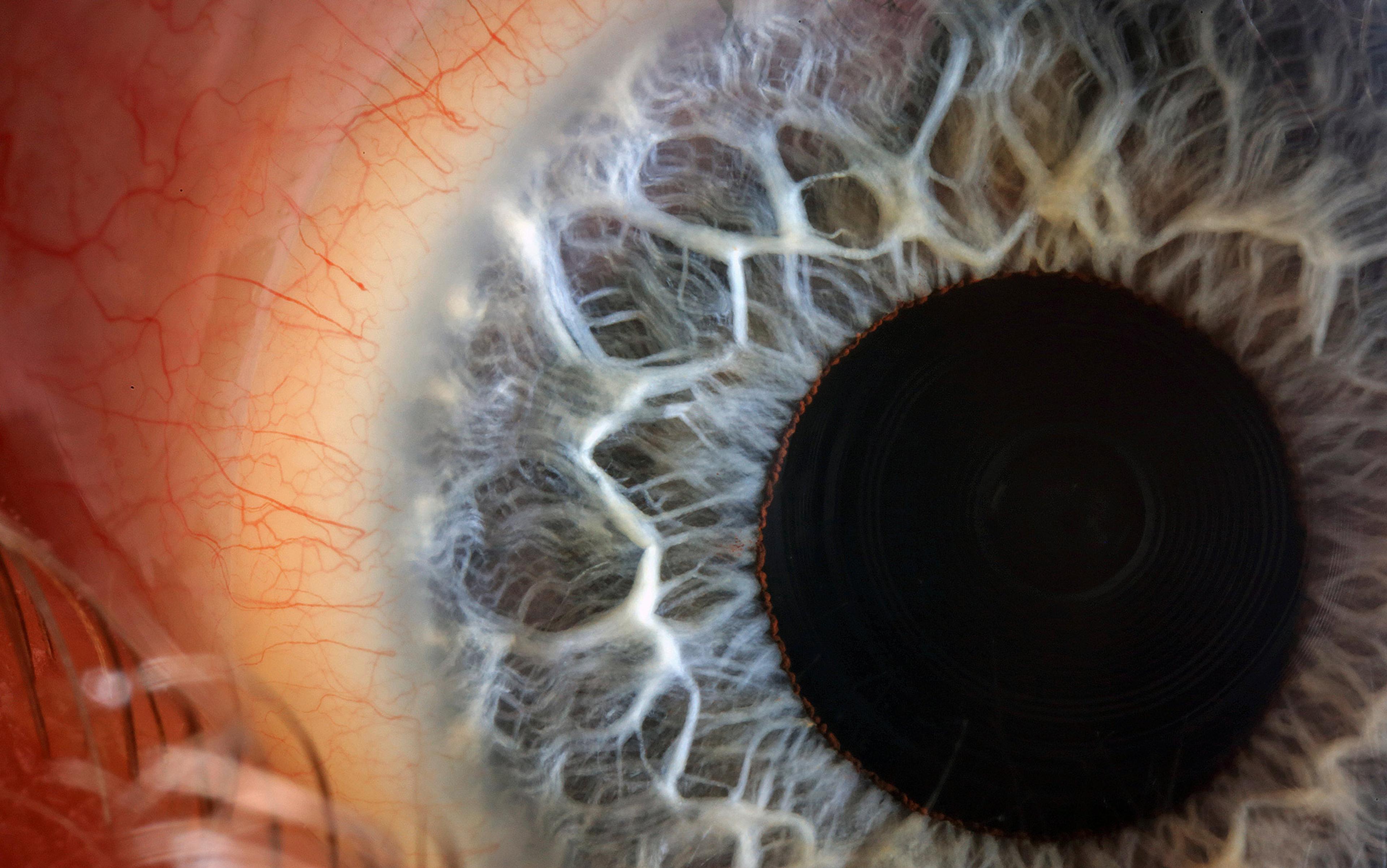
Thankfully, brain imaging has advanced quickly over the past decade – especially functional magnetic resonance imaging (fMRI), the process I described from the patient’s perspective above. This technology involves huge magnets that measure the flow of blood in different parts of the brain, a proxy for which areas are active at any given time. Using fMRI, researchers can create a map of an individual’s neural activity while thinking of a particular concept, such as ‘a spider’; by finding this brain pattern for people with phobias, researchers are then able to reduce the need for exposure during treatment.
How? Armed with a trace of an individual’s pattern for ‘spider’, it’s now possible to give patients positive reinforcement when they manage to reduce activity in the areas of the brain that correspond to the experience of overwhelming fear of spiders. Crucially, we can do this without ever showing them any eight-legged nasties. Instead, using the cue of a circle or a pleasant tone, and the reward of watching it change shape or pitch, the person themselves finds alternative means of subduing neural activity in these regions. In this way, the brain begins to modify its own internal states, and the phobia will subside as if by magic.
Not only is neurofeedback non-invasive; a number of high-profile research projects have also shown that it can be effective even when participants aren’t aware of the goal of the procedure. This new, unconscious reprogramming has far-reaching implications for research on human cognition, tapping into the crux of the mind-body connection, and opening up many new opportunities for novel clinical treatments. But it also has a potential dark side: the risk that neurofeedback could become a back-door for manipulating our brain states, without us even realising it.
The up-and-down story of neurofeedback research began in an unlikely way: with a story about NASA, lunar jet fuel, and hallucinating cats.
In the 1960s, the brain researcher Barry Sterman at the University of California, Los Angeles and his colleagues found that you could train cats’ sensorimotor rhythms just by giving them a bit of food every time they managed to activate a particular motor region. This was an example of Pavlovian or classical conditioning, where a creature learns a stimulus that triggers an involuntary response. It was one of the first demonstrations that this kind of conditioning could produce an effect on brain function, rather than just a behavioural reaction. Later, Sterman went on to conduct another study involving cats, observing the effects of lunar-lander fuel on mammalian systems for NASA. Most of his feline subjects became unsteady on their feet, the fumes beginning a slow degeneration that progressed through hallucinations, seizures and, eventually, death. But there were some extraordinary exceptions: the cats who had undergone brain-training seemed to be immune to the jet fuel’s degenerative effects. Somehow, each of these cats seemed to be able to regulate their neurological responses, and most recovered from the fumes. It was this finding that lead to the introduction of neurofeedback into NASA’s training programme, where it still plays a role today.
Around this time, the cognitive researcher Joe Kamiya at the University of Chicago began conducting some of the first formal studies of neurofeedback. Studies had shown that human subjects were able to voluntarily affect their heart-rate, skin temperature and sweat response. Kamiya demonstrated that, with the help of positive reinforcement (such as the sound of a bell), people could be trained to regulate their brain states in order to produce ‘alpha’ waves associated with relaxation. This was a form of operant conditioning – different to Pavlovian conditioning, because it was about learning to associate a voluntary behaviour, rather than a stimulus, with a particular reaction.
We’d seemingly found an intervention that was cheap, non-invasive, and wildly effective
Kamiya and his generation of researchers used a brain-imaging method known as electroencephalography (EEG). This involves placing a cap on the head, with a bunch of channels created by metal disks that are roughly a dime in diameter. They pick up electrical signals emanating out of the skull, and print them out as waves that provide information about how fast particular groups of neurons are firing together. In turn, these brainwaves can be linked to certain clinical conditions and brain states. For example, autism spectrum disorder is marked by excessive slow waves (delta) in the front of the brain. Separately, you can tell when someone’s eyes are closed because an alpha wave begins in the back of the brain and slowly creeps its way to the front. In the early days of neurofeedback, researchers would place this cap on a participant’s head and offer pleasant tones or a happy face on a screen whenever the read-out yielded brainwaves that would result in a positive clinical effect. It seemed to work, and neurofeedback had its first boom.
But there’s a technical problem with EEG: the signal it receives is a very grainy, global measure of brain activity. You can often find the same EEG signals from very different internal brain dynamics, many of which are not linked to intended clinical outcomes. The signal is so coarse, in fact, that it can be influenced by many non-neural signals, such as clenching your teeth and blinking your eyes. It’s far from perfect; however, it’s a cheap measure that’s still ubiquitous in the brain-imaging world.
As the first flood of neurofeedback research began, many early studies had positive results. We’d seemingly found an intervention that was cheap, non-invasive, and wildly effective. It wasn’t until the reproducibility crisis that we began to see a problem with this promising tool.
Reproducibility has become a huge headache for psychological research. In 2015, hundreds of researchers engaged in a joint effort to recreate 100 seminal psychology studies, 97 of which had originally produced significant results. When replicated, however, only 36 of the findings remained intact. There are many reasons for this crisis, but one of the biggest failings of traditional experiments in human behaviour has been underpowered design. Simply put, often there’s not enough data to determine whether the supposed effect you’ve observed is truly a fact of nature.
The problem was especially acute in these early neurofeedback studies. Not only were there too few participants to prove a real effect, but there were also likely to be serious self-selection biases among those who participated. People would often have to travel to clinical centres for several days or even weeks at a time, which meant that anyone who chose to do so probably shared certain features or were of a particular type. People who didn’t see a clinical difference often dropped out of the studies early on, whereas those who believed in the results would stay until the end of the treatment. These ‘believers’ might have swayed the positive outcomes in several neurofeedback studies.
So, what to do? Neurofeedback experiments often took many days – sometimes involving more than 20 training sessions – and the participants were always aware of the intended clinical outcomes. Looking back on these studies, many have not been replicated, while others have failed to show a difference when compared with a placebo.
Those initial studies of cats and jet fuel, or of bells and operant conditioning in human beings, were covered up by a swell of unconvincing findings. As a result, neurofeedback gained a reputation as a pseudoscience. The tidal wave of neurofeedback research quickly slowed to a trickle.
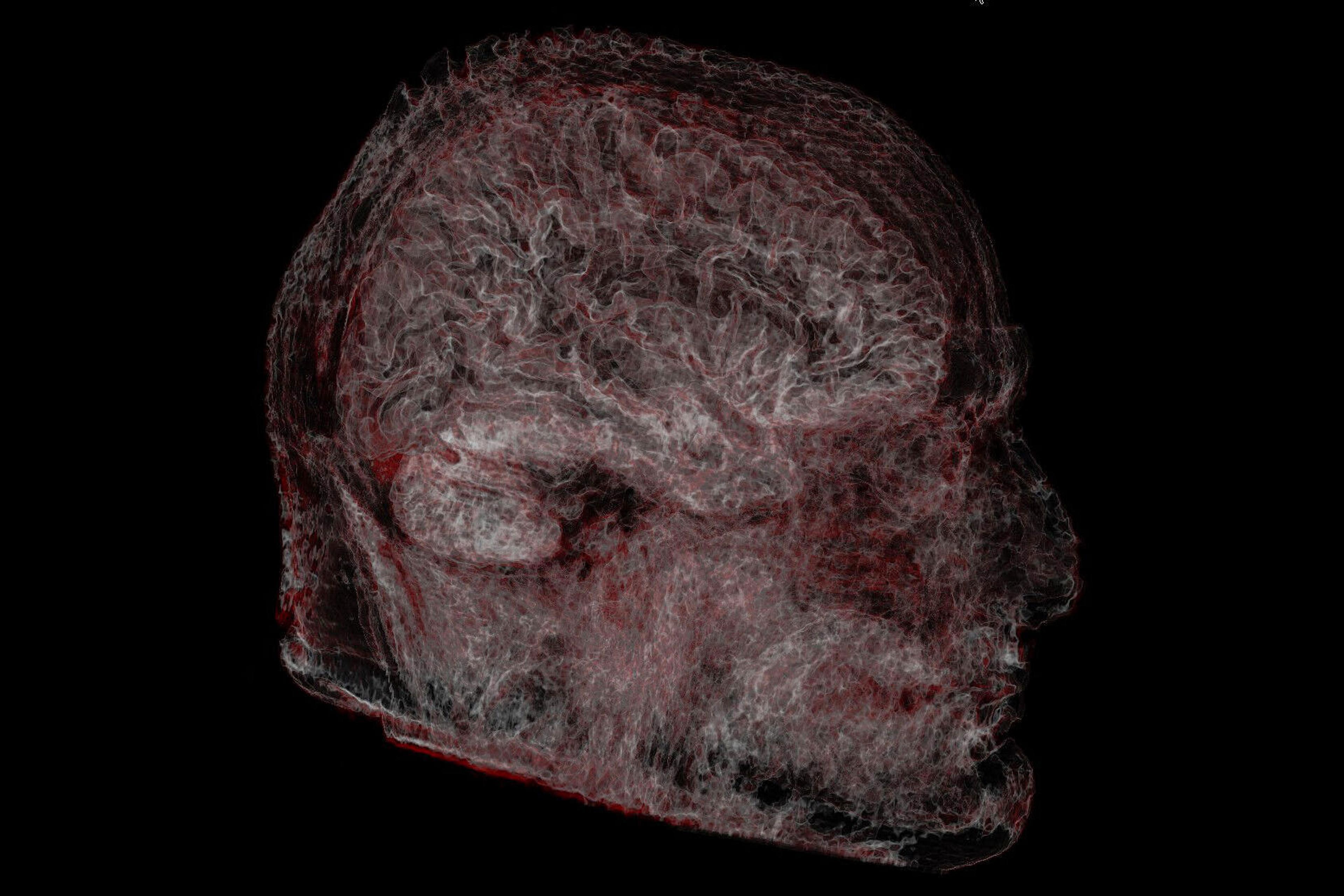
The better part of three decades passed until fMRI stormed on to the scene in the 1990s. Now, instead of vague information about brain states based on waves, we were able to derive 3D snapshots of exactly which brain areas are active during cognition.
You could create lasting change in brain activity just by thinking that you are undergoing an intervention
With this new technology in hand, researchers began trying to teach people to regulate specific brain regions. This was a major boost for neurofeedback. Not only could scientists make sure that they were creating the intended brain changes in their clinical interventions, right down to the specific cubic-millimetre regions they intended to train; but this same technology could also prove that the brain had undergone a profound change. Studies began to show that teaching individuals to regulate a single brain region in just a few clinical sessions could produce lasting changes in the way that brain region behaved – sometimes even months after the initial intervention.
Because these new forms of neurofeedback were much more localised in brain space, it took far fewer sessions to create neuronal modifications than in previous EEG studies – reducing training from a dozen or more sessions to four or five. However, this new brain-imaging method also proved something that no one had expected: you could also create lasting change in brain activity just by thinking that you are undergoing a real intervention.
The problem with neurofeedback is in fact as old as placebo itself. In double-blinded, placebo-controlled neurofeedback studies, neither the researcher nor the participant is aware of whether they are receiving a true intervention. When no one knows who is supposed to experience the clinical effect, the behavioural differences between placebo and neurofeedback intervention often disappear.
Even more impressively (or disturbingly), it seems that the mind can change the brain by just thinking it might be undergoing an intervention. New studies showed that giving people ‘sham’ neurofeedback could have the same effect as the real thing. When people believed they were undergoing an intervention, they usually reported feeling that it had a noticeable effect. Sometimes, the brain activity in these individuals also began to show the brain being retrained as intended: not only would participants of sham-neurofeedback experiments report reduced chronic pain, for example, but their insulas (the region of the brain directly tied to the experience of pain) would show a reduction of activity.
Since the early 2010s, neurofeedback has been fraught with this additional controversy. Researchers began to wonder whether all neurofeedback simply pertains to some deep, powerful capacity of the brain to change itself – and it needs no real technology to do it.
The placebo studies raise the question of whether you can really disentangle the mind from the brain. The Hollywood blockbuster Inception (2010) plays with a similar idea: in the film, the hero (played by Leonardo DiCaprio) alters people’s thoughts by jumping into their minds as they dream.
A new wave of research is focused on a brain imaging technique so similar that its advocates have called it ‘incepted neurofeedback’. These studies show it’s possible to implant thoughts into people’s brains without them being aware of it. In one case, researchers scanned participants to get a ‘baseline’ reading of their brain activity, and then subjected them to several days of neurofeedback training. When subjects saw black stripes on the screen, they were instructed to ‘somehow regulate [their] brain activity’ to make a grey circle in the centre of the screen get as large as possible. At the end, they got paid money depending on how successful they were. What they weren’t told is that the size of the circle was related to patterns of brain activation that corresponded to seeing the colour red.
After doing this hundreds of times, people were asked what helped them get high scores. No one mentioned colours; some mentioned zebras, violent acts or performing in gymnastics tournaments. In subsequent tests, though, the participants were more likely to see the colour red when presented with an image than those who didn’t receive neurofeedback. Without even knowing it, the visual mark of ‘red’ had been implanted in their minds.
Research by the psychologist Vincent Taschereau-Dumouchel at the University of California, Los Angeles, and colleagues have applied this technique to phobias. In a study published in 2018, they recorded the brain activity in ‘normal healthy participants’ while they experienced certain cognitive events, such as looking at pictures of a spider or snake. They then averaged out this brain activity, giving researchers a template or ghost signal of the underlying brain activity associated with these animals.
It’s a remarkable advancement, but the clinical and ethical implications have barely been explored
With this signal in hand, the researchers then brought in someone who has a phobia of spiders or snakes. Using neural-reinforcement mechanisms such as the changing circle, they never exposed participants to their fears or even told them if they would experience reduction in their fear response. The process was completely unconscious. Nonetheless, over several days of training, these subjects successfully reduced the brain activity associated with those cognitive events, and showed a smaller physiological fear response (based on sweat and activation of the amygdala) when finally shown an image of their fear.
This clever new approach has found a way around the placebo problem. Participants have no awareness of what’s being done with the intervention; consequently, the brain changes observed in these studies are undeniably tied to the training of brain activity. The people involved also avoid negative reactions that come from being exposed to their fears.
While the outcome is a remarkable advancement for neuroscience, the clinical – and ethical – implications of such methods have barely been explored. If it proves to be robust, neurofeedback could be revolutionary for patients with otherwise intractable disorders, such as schizophrenia, locked-in syndrome, even dementia. We can expect to see studies in these areas popping up in the coming years. Neurofeedback is even coming into its own as a mechanism for affecting higher-order cognition: rather than a simple up-or-down regulation of a particular brain region, one study has even demonstrated that neurofeedback can be used to change levels of confidence. With this newfound opportunity to reprogram patients’ brains with varying levels of conscious awareness, it’s important to reflect on how incepted neurofeedback could be abused in the wrong hands.
When it comes to the clinical future of fMRI neurofeedback, we’re simply in uncharted waters. As it becomes more widely used as a psychological tool, the nature of consent clearly needs to develop. In most clinical research, you are made aware that you might either be in the ‘active’ or the ‘control’ (ie, placebo) condition, so you never know if you are receiving the intervention that you’ve been briefed on. But what if there is medical benefit to entering an intervention without any bias caused by expectation? Some incepted studies have addressed this issue by gaining consent from legal guardians, in which someone who is not receiving the treatment at least knows the full story of what’s going on. At least one thing seems certain: if neurofeedback is to reach its potential, it demands we think carefully about the scientific and philosophical basis of human agency.