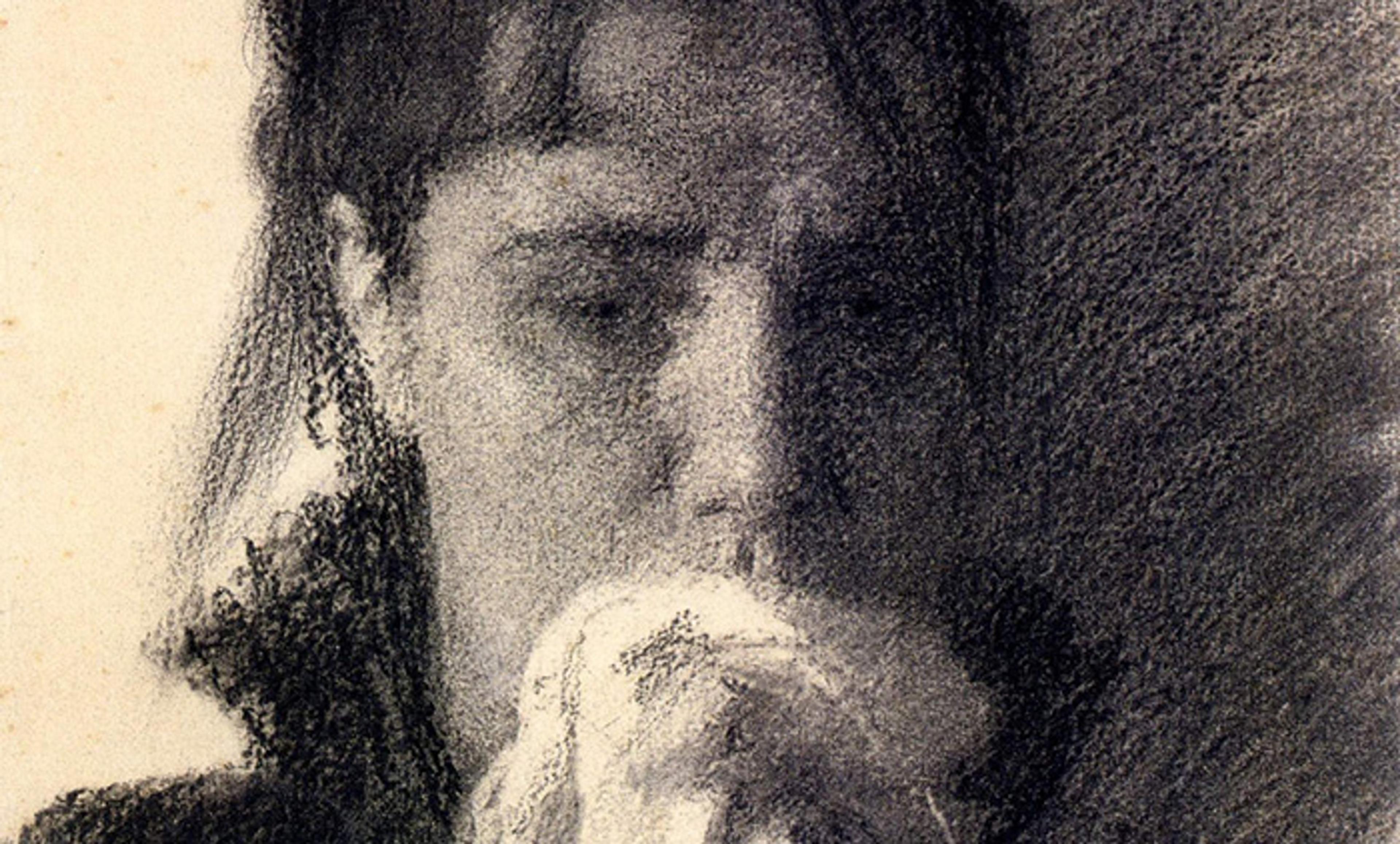
Detail from study for the painting Inconsolable Grief (1884), by Ivan Kramskoi. Courtesy the National Museum, Kiev
It’s a tragic fact of life that most of us will experience the loss of a loved one. Approximately 50 to 55 million people die worldwide each year, and it is estimated that each death leaves an average of five bereaved individuals. The experience of loss usually causes a range of psychosocial reactions, such as withdrawal from social activities, deep sadness, confusion about one’s role in life, and bursts of loneliness. In the acute phase of bereavement, these types of grief reactions are often all-consuming, excruciatingly painful, and highly impairing. It can feel as if the love directed towards the deceased person suddenly loses its tangible object, leaving the bereaved individual with an intense emptiness.
Thankfully, over the longer term, most people, most of the time, have sufficient resources to adjust to their new life without the person they’ve lost. They don’t necessarily ‘get over’ their loss, but they learn to cope. Sadly though, this isn’t true for everyone. Accumulating research within psychiatry and psychology has shown that a significant minority of people – approximately one in 10 – do not recover from grief. Instead, the acute reaction persists over the longer term, leading to trouble thriving socially, mentally and physically.
The distinction between the typical and the more problematic version of grief can be illustrated through an analogy. Much like a physical wound usually heals on its own, even if it is painful and slow, most people recover from their grief without any specialised help. However, occasionally, a physical wound becomes inflamed, and we use ointments, creams and patches to aid the healing process. Similarly, complications can sometimes arise in the grief process, and extra help is then necessary to treat the ‘inflamed’ grief.
An intricate mix of individual and contextual factors can lead to the development of complicated grief reactions. Imagine Amy, a 50something woman living a quiet life with her husband and two teenage sons. While out for a jog, her husband has a sudden heart attack and falls to the ground. He receives cardiac massage from a passerby but is declared dead at the local hospital hours later. This hypothetical experience could initiate very different paths of grief for Amy. In one scenario, we see an Amy who is profoundly affected by the loss in the acute period of grief. She uses an immense amount of time and energy to prepare the funeral, sort her deceased husband’s belongings, and adjust to life as a widow. Her workplace is very understanding of her situation as both her colleagues and supervisor support her and put arrangements in place to manage her absence. She works hard at getting her life back on track to give her children a happy childhood. Five years after her loss, she is highly engaged in an organisation working with the prevention of heart diseases. She still misses her husband tremendously, but she is grateful for the years they spent together.
Conversely, the shock and the trauma of her husband’s death could send Amy on a different path: she struggles with accepting the permanence of the loss and, even years after his death, keeps all her husband’s belongings untouched; her employers are unsympathetic, and she loses her job due to too many sick days and decreased work performance; and her continued low mood and lack of energy lead her friends and relatives to withdraw. In this scenario, Amy is unable to meet the demands of her sons, provoking loneliness, frustration and self-loathing; she shows no interest in the outside world, and is overwhelmed by an intense sadness that doesn’t decrease over time.
These contrasting hypothetical scenarios illustrate how susceptibility towards grief-related complications can vary depending on key factors (eg, level of social support, personal coping style, attainment of new interests after one’s loss). If a person experiencing complicated grief doesn’t receive appropriate support, further adverse consequences can develop, such as heightened risk of serious health conditions, impaired quality of life, and lower general functioning.
Research attesting to the distinctiveness of persistent grief and its associated adverse effects led the World Health Organization (WHO) in 2018 to decide to include a grief-specific diagnosis in their classification guidelines for mental disorders, known as the ICD-11 (International Classification of Diseases, 11th revision), which will be fully implemented in healthcare systems by 2022. The new diagnosis, termed ‘prolonged grief disorder’, is characterised by an intense longing for, or a persistent preoccupation with, the deceased, accompanied by intense emotional distress (such as blame, denial, anger, difficulty accepting the death, feeling one has lost a part of one’s self) and significant impaired functioning that persists beyond half a year after the loss.
As the ICD-11 begins to be implemented in the coming years, there is a need to disseminate information on the diagnostic criteria of prolonged grief disorder to healthcare professionals who are in contact with bereaved individuals at hospitals, hospices, intensive care units, and to general practitioners, to help them identify and offer appropriate support to those who need it. Unfortunately, media headlines about the new ‘grief-diagnosis’ can imply that prolonged grief disorder considers all kinds of grief reactions as pathological. This is rather unfortunate as it might cause some individuals to hide or avoid their grief in an attempt not to receive a diagnosis. Also, preventive interventions directed toward normative grief reactions can be both ineffective and even contraindicated, making it vital that prolonged, complicated grief is not overdiagnosed.
The diagnostic guidelines developed by WHO are used by psychiatrists and psychologists throughout most of the world, and the addition of prolonged grief as an official mental disorder has several practical implications. Earlier, symptoms of prolonged grief disorder were often interpreted as signs of depression and treated by antidepressants, but these types of drugs have shown minimal effect in ameliorating grief symptoms. The recognition of prolonged grief disorder as a distinct phenomenon will hopefully ensure the appropriate allocation of effective psychosocial treatments.
Such approaches include an element of psychoeducation: informing the client of the healthy and more pathological versions of grief, and discussing therapeutic goals. People experiencing complicated grief often avoid people, situations or objects that remind them of the permanence of their loss, so some version of exposure is often used. Exposure might include retelling the story of the loss or identifying particularly disturbing memories that the person tends to avoid, and then gradually revisiting these memories within and between treatment sessions. The final stages of therapy are often future-focused, working towards resumption of life without the deceased. This element emphasises establishing and maintaining a healthy bond to the deceased, including an acceptance that life continues, and targeted help to reengage in meaningful relationships.
The saying ‘time heals all wounds’ is only partially correct because, for severely inflamed wounds, time is not the solution. It is necessary to see a doctor and receive specialised treatment to aid the healing process. Bereaved individuals experiencing complications in their grief process often describe their situation as extremely numbing, overwhelming and debilitating. As shown in the case of Amy, one’s social network is a crucial factor. While an understanding and supportive network can act as a protective factor against prolonged grief disorder, withdrawal from friends and family can create social isolation and increase feelings of meaninglessness, contributing to the development of prolonged grief disorder. It is essential to know that professional help is available. If you read this and recognise the symptoms of prolonged grief disorder in someone you know – or perhaps in yourself – seek out professional support because time does not heal all grief.