‘Psychosis’ is a blanket term for a range of symptoms related to losing touch with objective reality, including hallucinations and delusions. People with psychosis feel as if their unusual experiences are real, but the way they make sense of them varies hugely. Crucially, the extent to which they realise that their experiences are due to illness – that is, how much they have ‘insight’ – affects their chances of recovery, and interventions aimed at increasing insight are showing great promise.
Consider the (fictional) case of John, a 24-year-old man who began hearing a voice speaking to him, and interpreted it as part of a sinister organisation determined to steal his ideas. His concerned mother sought professional help after he withdrew to his room for days on end and, after refusing treatment, John was eventually admitted to a psychiatric hospital under a section of the UK’s Mental Health Act (1983).
In one version of this story, John continues to maintain that there is nothing wrong with him and he wants to go home. He is still ‘hearing voices’ and explains that the people responsible have followed him into the hospital using the internet. When asked for evidence, he simply says he knows it to be true. He believes he doesn’t need medication, which he says is likely to contain poison. His psychiatrist would, hopefully, understand the degree of distress and fear that John is experiencing, and will try to find some way to win his trust, but he will also conclude that John’s insight into his illness, his symptoms and his need for treatment are completely lacking.
By contrast, in a version of the story in which John has good insight, John begins to wonder whether his mind is playing tricks on him. He reasons that perhaps he is very ‘stressed’ and, because of social and sensory isolation, he is having hallucinations (even though they seem real). He recognises that he is in a bad way and needs help. Though not sure what can be done, he at least feels safe in hospital. The medication seems to be making him calmer, and he feels more trusting of those around him – he is happy to keep taking it. He wonders now whether the ‘conspiracy theory’ was over-the-top. John’s appraisal of his situation and ability to consider alternative explanations of his experience leads his psychiatrist to deem him to have good insight.
Thirty years ago, working as a junior psychiatrist on inpatient wards in London, I was struck by the vast range of attitudes that patients had to their psychotic experiences. While some were utterly convinced of the reality of their hallucinations and extreme beliefs, just like the first version of John, others were more similar to the second version, open to the possibility that there might be other explanations for what they were experiencing, such as stress or illness.
These observations inspired me to write my first paper on the topic of insight, in the British Journal of Psychiatry in 1990, where I proposed a working definition. I argued that insight in this context has several dimensions, including: a general appreciation that one is unwell, sick or changed, and that this is a biomedical matter rather than a moral or religious one; an ability to relabel unusual sensory experiences and beliefs as pathological; and, finally, acceptance of treatment.
My paper went against the prevailing dogma that people with ‘neurosis’ (milder forms of disorder such as anxiety and depression) can have insight whereas those with psychosis never do. An anonymous editorialist for the prestigious medical periodical The Lancet commented at the time that studying insight was ‘academically nourishing but clinically sterile’. Torn between feeling flattered by the attention and insulted by the judgment, I persisted researching the topic, convinced that increasing our understanding of insight could help us better support those who find themselves unable to accept the help and treatment that we sincerely believe to be in their best interests.
Decades later, we now have some ‘facts’ about insight in psychosis. Importantly, it can be measured in ways that are at least as valid and reliable as for any other recognised psychopathological phenomenon. We’ve also discovered some well-replicated and important associations, above all that poorer insight correlates with more serious mental illness.
That might seem obvious, but the relationship is not 1:1 – some people can have very severe symptoms and good insight (and vice versa), but the two factors do tend to move in the same direction. Lower insight also correlates with lower IQ. Again, it is not a simple correspondence, but the ability to generate hypotheses and a new angle on what one is experiencing is helped by better intellectual functioning. Perhaps more surprising is that lower insight also correlates with better mood. Some experts believe that this is because having insight into one’s predicament – especially if it is challenging – is bound to cause depression and demoralisation. While this is likely to be a factor, research suggests that the direction of causality is not one-way. Having a low mood might also enhance the ability to see the world more accurately and objectively, including one’s own mental state – known as ‘depressive realism’. Finally, there is the more obvious and clinically relevant relationship between better insight and greater treatment adherence, and hence better outcomes.
The study of insight in psychosis has not been without controversy. The link between poorer insight and the need for more coercive treatment is, naturally, where critics of the insight concept converge. ‘Insight’, they say, is merely agreeing with the doctor. Yet what else can we call it but lack of insight if a patient considers himself well and in need of no help while his caring peers and loving family argue exactly the opposite?
Ethical questions surrounding insight play out perhaps most vividly in relation to legal judgments of a person’s ability to ‘use and weigh’ information, a key criterion for ‘mental capacity’ as defined by the UK’s Mental Capacity Act (2005). This legal Act, which sets out the requirements for people to be treated against their will, states that a person lacks capacity if, as well as being unable to retain information and communicate a decision, he is unable to use and weigh (or appreciate) relevant information to come to a decision. This is where the concept of clinical insight comes in – it is hard to see how the benefits and harms of a proposed treatment can be weighed in the balance if you don’t believe you are ill in the first place.
I believe strongly that restoring or improving insight is a worthwhile aim of psychotherapy, helping to increase the chances of a patient’s recovery. It should be in the form of acknowledging difficulties as a first step in gaining mastery over them. Then, as a next step, encouraging openness to take up an effective treatment for distressing symptoms, not forcing the patient to accept some abstract illness model. This was the approach of the now retro-sounding ‘compliance therapy’ trials that my colleagues and I conducted in the 1990s, in which a brief intervention, involving educational components and guided problem-solving, led to promising results in terms of greater acceptance of drug treatments.
More recently, a range of talking therapies have been designed that use visual illusions and other exercises to show patients that first impressions are not always correct and that you can’t always believe your eyes, with the ultimate aim of improving their general ‘metacognition’ (that is, their ability to reflect upon their own cognition). Studies using this approach, often involving patients with a range of mental disorders, have also reported promising results, though the implications for improving clinical insight per se are not yet clear.
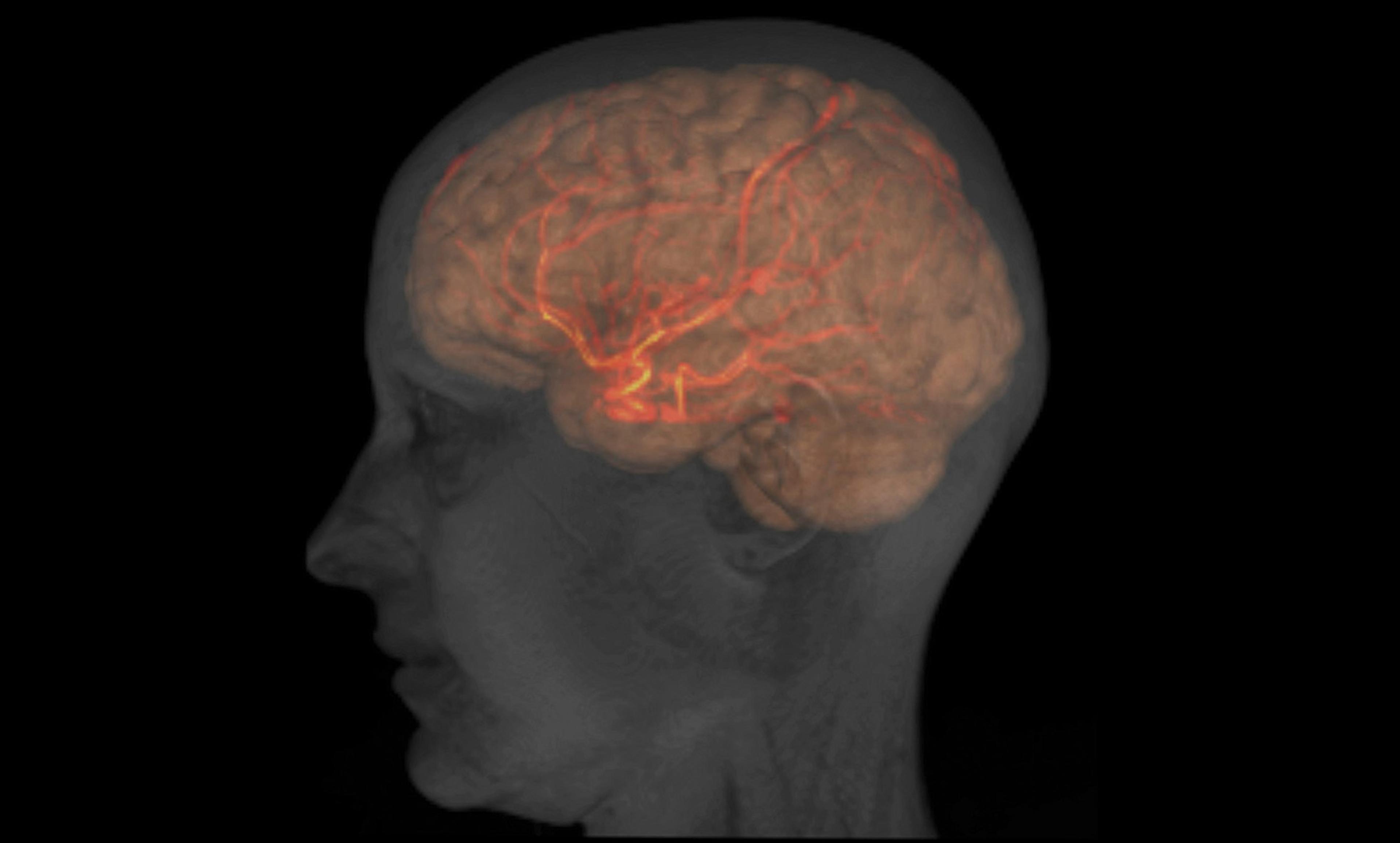
Another exciting avenue of research involves using transcranial direct-current stimulation (tDCS) to safely and noninvasively modulate neural activity in targeted regions of the brain. It would be simplistic to suggest there was an ‘insight centre’ in the brain, but systems and networks have been identified that are active during self-appraisal – the so-called cortical midline system. Research with elderly volunteers showed that tDCS over a region connected to this system (the dorsolateral prefrontal cortex) increased their awareness of their own errors in computer-based tasks. Building on this, a pilot study in 2014 showed that tDCS to the same brain region increased clinical insight to a small but statistically significant extent in a group of patients with schizophrenia (we must wait to see if this finding can be replicated in a controlled trial).
Looking back, there has been a great deal of activity around the topic of insight since my first foray into the area. Much of it has been therapeutically orientated, while other work on metacognition and related concepts has also shone a light on profound, universal aspects of human psychology – such as self-knowledge. Contrary to the claims of my early critics, the study of insight has proven to be both academically simulating and clinically fertile. It is a biopsychosocial construct par excellence. I am looking forward to what new insights the next 30 years will bring.
For readers wishing to find out more, I published a more detailed account of the past 30 years of research into clinical insight as a comment piece in the British Journal of Psychiatry.