‘As long as it’s healthy!’ Up until now, this cliché was merely a generic – if somewhat ominous – way for expecting parents and their loved ones to talk about their future children. But what if that outcome was not merely an expression of wishful thinking, but something that parents could control? Imagine a fertility doctor examining the embryos that could develop into your children, providing you with a menu. One has a heightened risk for schizophrenia but a very low risk for cancer; another has relatively low risks for these diseases but a three-fold increased risk for Alzheimer’s disease; and a third has roughly average risks for all of these diseases. Oh, and the first two are boys, while the third is a girl.
While this may sound like a science-fiction movie, several private companies have begun selling services that resemble this scenario. Such companies cater to couples undergoing in vitro fertilisation (IVF), offering to generate a genetic risk profile for each of their frozen, days-old embryos. It’s estimated that more than 100 families have already taken these tests, and some resulting babies have been announced. But is it really possible to offer such a ‘menu’ in a way that provides meaningful, scientifically valid information? This question has been the focus of our work as geneticists in the past few years. To the extent that the answer is yes, it raises an even more challenging question: should this be allowed?
To better consider these questions, we’ll review some key arguments for and against this kind of risk profiling – called ‘polygenic embryo screening’, or PES. (Terminology in this new field is not fixed, and the procedure is also sometimes called ‘preimplantation genetic testing for polygenic diseases’, or PGT-P.) We will attempt to clarify which arguments are relevant and convincing, and which require further study. We will also consider this technology in the context of the historical evils of eugenics. Since the word eugenics is too often used in a manner that sheds more heat than light in discussions of genetic technologies, we will first lay out what is known (and not yet known), before engaging with the most inflammatory aspects of the debate.
Despite ample initial scepticism, recent science has demonstrated the potential utility of profiling human embryos for disease risk. Importantly, if these profiles are used to select the ‘healthiest’ embryo from a given IVF cycle, the child to be born is expected to have better health than a randomly selected sibling embryo. However, unbridled enthusiasm would be misguided: these bright predictions might only be fulfilled under certain conditions, and there is a risk that consumers using these services will be misled about their benefits. Further, widespread implementation of embryo screening will not only complicate IVF clinical procedures, it could also have social and psychological effects that reverberate far beyond the clinic.
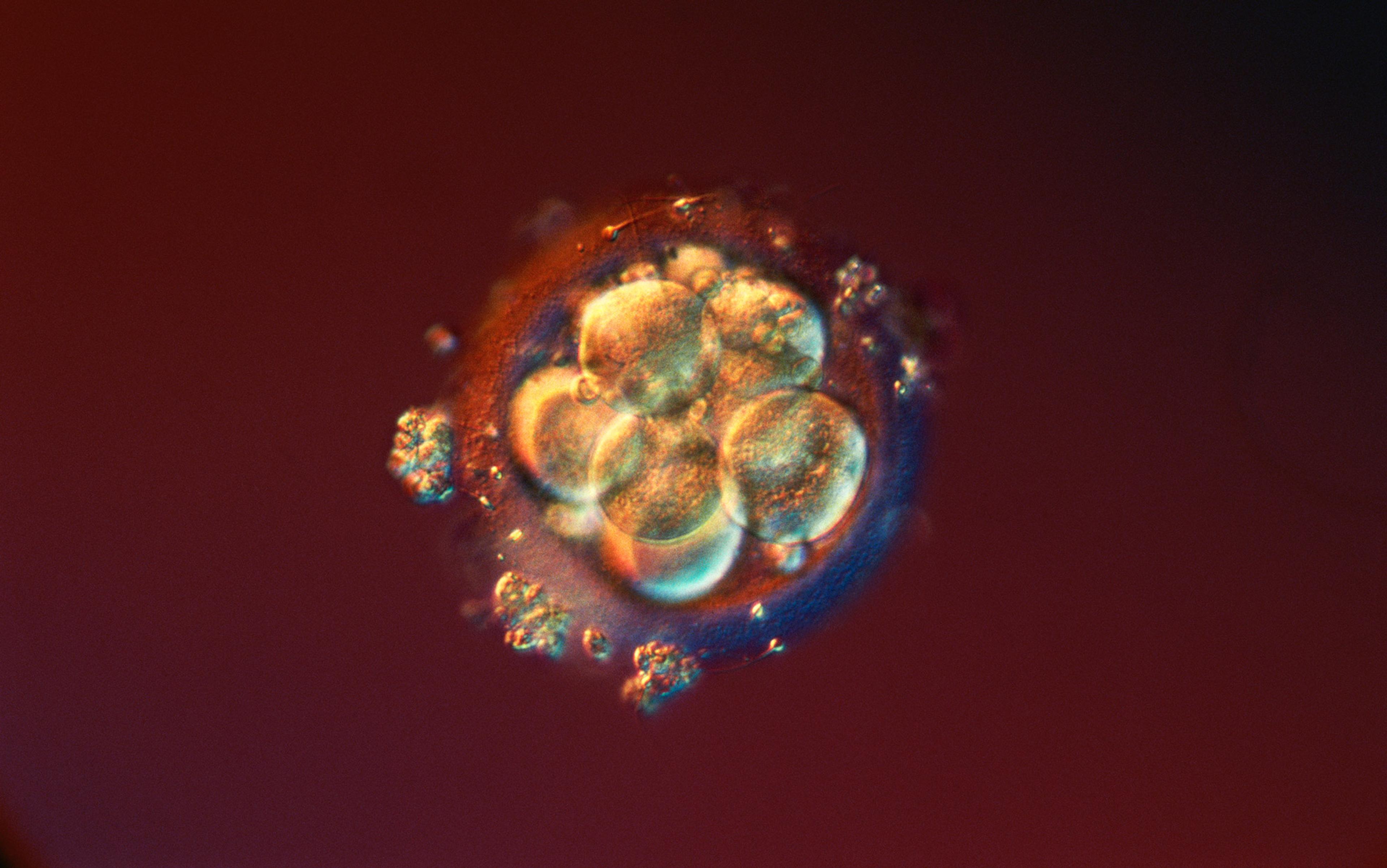
Since in vitro fertilisation was introduced in the late 1970s, more than 8 million children have been born using the process. During IVF, multiple eggs from the intended mother (or a donor) are fertilised by the sperm of the intended father. While fertility issues cause many couples difficulty in becoming pregnant, it is still common that multiple viable embryos are available. To decide which embryo should be transferred into the uterus of the mother, embryologists typically pick one based on morphology – the physical appearance of the embryo under the microscope, which can be suggestive of healthy development.
In some IVF cases, the parents carry a genetic mutation that, if transmitted to the child, will lead to a severe early childhood disease (for example, cystic fibrosis). In these cases, an embryo is selected based on its DNA. A tiny biopsy of just a few cells is taken from the developing embryo, DNA is extracted from the cells, and only mutation-free embryos are considered for transfer. This form of preimplantation genetic testing (PGT) has been available for more than three decades, but it is irrelevant to most potential IVF parents, since only a minority of parents carry these rare mutations.
The new services, however, are potentially relevant to all parents: they offer testing for the common diseases of adulthood, including heart attack, stroke, diabetes, various cancers, Crohn’s disease, schizophrenia, depression, Parkinson’s disease, and Alzheimer’s disease, among others. Common to these diseases is that they are polygenic: there is no ‘one gene’ for, say, heart attack. Beyond other risk factors such as diet or exercise, heart-attack risk is influenced by thousands of genetic variants scattered throughout the genome. The risk attributable to genetic factors that a person (whether an embryo or an adult) will have a heart attack in their lifetime can be computed with what’s called a polygenic risk score. This score is interpreted as a probability, so the prediction is uncertain: a person with high estimated risk may end up not having a heart attack. This differs from the typical scenario for PGT, where having the relevant mutations will cause the disease (eg, cystic fibrosis) with near certainty.
A key question about this newer form of screening, which has been available to consumers since 2019, is whether it can lead to a meaningful improvement in the health of the child to be born. The answer seems to be affirmative. Using statistical models and simulations, we and our colleagues have shown that selecting the embryo with the lowest risk for a given disease can cut the risk for that disease by almost half, at least in the best-case scenario. This is particularly true for disorders such as schizophrenia and Crohn’s disease, which are relatively uncommon in the general population and are strongly influenced by genetic risk factors. Other simulations show that when embryos are ranked by their combined risk for 20 diseases and the best-ranking embryo is selected, the risk for most diseases drops by roughly 5 to 20 per cent. These results address initial concerns that risk prediction is not sufficiently accurate, or that the embryos are not sufficiently genetically different from one another, or that reducing the risk of some diseases will increase the risk of others.
Will intended parents correctly understand the probabilistic nature of disease-risk prediction?
We remain sceptical, however, that this approach can lead to meaningful improvements in non-disease traits such as intelligence. Our research has shown that the statistical uncertainties are too large when predicting such traits, and are expected to remain large for the foreseeable future. For example, if selecting from a batch of five embryos, the one predicted to have the highest intelligence would, on average, have an IQ only 2.5 points higher than a randomly selected sibling. More importantly, that average prediction would be surrounded by a margin of error of at least ±15 points, meaning that the selected embryo could develop to be far less intelligent than predicted.
What’s more, despite the optimistic projections for disease-risk reduction, we expect these reductions to be more modest in practice than predicted, for three main reasons. First, many couples will not have a sufficient number of embryos to choose from. It is well known that IVF is not always successful. Our calculations were based on the availability of five viable embryos, which is unrealistic for many couples, particularly older ones. Second, polygenic risk scores are based on genetic analyses of adults with a given disease, derived from very large, expensive genetic studies primarily conducted in Western countries with individuals of European descent (eg, white American and British individuals). Risk prediction is much less accurate in individuals of non-European ancestries, so PES will be less useful in these populations.
Third, it is unclear whether our current risk estimates will remain equally accurate decades from now, when environmental risk factors may be very different. For example, genetic risk for smoking is one of the greatest predictors of healthy lifespan in older individuals today; will the same be true for those born today, now that smoking rates are drastically lower than they were 50 years ago? Changes in dietary habits, new developments in medicine, or even future pandemics might impact the relationship between genes and health over the lifespan of the currently unborn.
Even if best-case estimates of risk reduction are achievable, it is important to emphasise that these refer to relative risks. Schizophrenia has a prevalence in the general population of approximately 1 per cent (at most). If embryo screening that targets schizophrenia risk provides a 50 per cent relative risk reduction, this translates into a 0.5 percentage point reduction in absolute risk. What started as a 99 per cent chance of being disease-free increases to 99.5 per cent, which sounds considerably less impressive than a ‘50 per cent reduction in risk’. There are numerous ways of communicating risk, each mathematically equivalent but leading to distinct differences in subjective impressions. This fact has led to guidelines for communication across all areas of general medical practice – but, unfortunately, these seem to be more honoured in the breach than the observance.
With such a complicated landscape of risks and benefits for PES, it is hard to foresee how couples will receive it. Will intended parents correctly understand the probabilistic nature and statistical basis of disease-risk prediction, including the caveats that may reduce the accuracy of prediction in their specific case? Will they easily see the distinction between relative risk reduction (which will likely be advertised by service providers) and absolute risk reduction, which can be very small for less-common diseases? Given that people are generally wired to find probabilistic reasoning counterintuitive, we have our doubts. And where there is an absence of regulation, as is the case in the United States, we are concerned about whether providers will offer this information transparently. If PES becomes widely applied, the shortage of genetic counsellors might further reduce the ability of prospective parents to fully comprehend the nuances of the procedure.
Concerns about PES don’t stop at debates over expected risk reductions. Issues related to psychological wellbeing, social values and ethics, while perhaps less tangible, are also vital to understanding the potential impacts of this procedure.
By situating prospective parents in the role of consumers – ‘choice over chance’ is the slogan of one company – PES raises concerns about the more insidious effects of consumer capitalism. The behavioural science concept of the paradox of choice suggests that, when there are too many perceived options, people tend to feel increasingly stressed by the decision and dissatisfied with whatever choice they make – fearing that one of the other options might have been better. The example of the dating app Tinder amply demonstrates that this phenomenon extends to commodified human relations. The idea that there are ‘plenty of fish in the sea’ used to be a source of optimism after a dating rejection, but now it is more often a source of dissatisfaction and reduced self-esteem when one is presented with too many potential partners.
Taken to the extreme, the experience of ‘choice overload’ might lead to the avoidance of making any decision at all. In the first public report of a PES case, five embryos were generated. Despite the fact that three embryos showed normal risk for all of the diseases tested, the couple elected not to implant any of the embryos and deferred the process to an unspecified later date. Similar outcomes were reported again and again.
While the focus of our research (which is partly funded by the US National Institutes of Health) has been on the statistical and medical properties of PES, we recognise that there is a serious need to study its potential psychological impact. To take another example: the genetic report will be the parents’ first impression of their unborn child. Will this first impression serve as an unshakeable anchor to their expectations for the child’s life? Could it even lead them to shape their child’s upbringing accordingly? For instance, we can ask whether a prediction of reduced risk for cardiovascular disease might lead a child’s parents to maintain a less healthy environment, one in which exercise and diet are not considered important – thereby cancelling out any health benefit derived from genetic selection. There is already experimental evidence that individuals who are told that they are at low genetic risk of obesity are more likely to choose unhealthy foods and deprioritise exercise. What if the parents have selected for reduced risk of psychiatric illness? Would that lead to a false sense of security, leaving them less attuned to potential signs of psychological distress in their child?
Routine knowledge of individuals’ genetic predispositions risks a redefinition of selfhood
We should also consider the children’s own self-perception and self-acceptance. In the sci-fi movie Gattaca (1997), three characters who have been ‘genetically assisted’ to be born with superior traits are each incapable of psychologically accepting their own limitations and failures, ultimately leading to the suicide of one of the characters. What is going to be the psychological impact of knowing, at an early age, that your own genetic risks have been quantified, and even ‘optimised’?
Currently, the American Medical Association and other professional organisations tend to counsel against genetic testing in minors for severe adult diseases, especially when there is no available treatment. This guidance follows from an assumption that children possess a ‘right not to know’ and are entitled to an ‘open future’, with freedom to shape their life unburdened by genetic expectations. The very limited research on children and parents to date suggests that receiving genetic testing results indicative of future disease risks leads to increased worry in some children, especially if there is a parental or family history of the disease. That being said, some have argued that fears of psychological harm of genetic disclosures to children are overblown, and that the right not to know should be weighed on a case-by-case basis.
While the extent to which preimplantation genetic screening will spread is difficult to predict (and the financial and emotional costs of the IVF process may be limiting factors), genetic testing is likely to become increasingly integrated into pregnancy and childbirth. In turn, many individuals may become aware of their own risk scores at very early life stages, whether or not they were selected and born using IVF. Given that we still lack systematic data concerning the way that adults perceive and react to information about their own polygenic risks, the perspectives of children and parents towards this kind of information will require intensive study and public conversation – preferably before PES becomes a more commonplace procedure.
One risk of genetic information is the tendency of many people to overvalue and reify genetic predictions, in a process called genetic essentialism. While genetic influences on most traits are probabilistic and partial – with considerable room for environmental and even random factors to ultimately influence outcomes – it is common for people to interpret genetic information as fully causal and definitive. This can lead to genetic fatalism, the belief that genetically influenced features are inalterable. In the context of widespread genetic essentialism and fatalism, routine knowledge – not to mention selection – of individuals’ genetic predispositions risks a redefinition of selfhood and individuality.
As geneticists who study psychiatric disorders, we recognise that genetic essentialism becomes especially worrisome in connection with mental health. Lack of agency and self-confidence is a common correlate of mental health problems; recent research has demonstrated that receiving genetic results indicative of risk for mental illness can lead to reduced self-confidence, with a concomitant negative impact on mood. Worse still, people may also be led to believe that their mental health problems are untreatable due to genetic fatalism. In the absence of clear communication and education about the limits of genetic prediction, genetic assessments indicating increased risk could lead to a vicious cycle of reduced self-worth.
Because psychiatric conditions are, arguably, the most stigmatising in our society, widespread early genetic testing could have broad ripple effects beyond families who use PES or otherwise elect to receive early genetic results. While scientists had hoped that biological explanations of mental illness might reduce stigma by drawing similarities to less stigmatised medical disorders, surveys suggest there has been only limited change in societal attitudes towards mental illness as a result, despite increasing acceptance of biological factors. A rising tide of testing, combined with genetic essentialism, could lead to an increased sense of pessimism about and stigmatisation of individuals suffering from mental illness, even those not tested. Research has indicated that increasing awareness of biological causes of mental illness may actually result in an increase in the perceived dangerousness of mentally ill individuals. Moreover, research has shown that clinicians are not immune to feelings of stigmatising pessimism, which could reduce their effectiveness in helping those with mental illness.
Viewed from this perspective, it is perhaps no coincidence that the American eugenics movement of the early 20th century heavily targeted those with psychiatric and cognitive disorders, leading to forced sterilisations of tens of thousands. Consequently, the spectre of eugenics has been a major concern associated with PES since day one.
Parents may feel compelled to make reproductive decisions that do not align with their values
Of course, the development of PES by no means necessitates a coercive use of state force. Indeed, some might suggest that the word ‘eugenics’ is unfairly applied to PES. By this argument, a freely chosen procedure such as PES is no more eugenic than any other long-established selection procedures utilised during IVF, such as preventing cystic fibrosis and chromosomal abnormalities, reducing breast cancer risk by selecting embryos without a BRCA variant, or even ranking embryos by their appearance under the microscope. Since an embryo must be selected anyway, this argument proceeds, why not use all available information? In societies that place a high value on reproductive autonomy, this libertarian argument may be compelling to some.
However, if increasing numbers of couples who can reproduce naturally begin to seek IVF services that include PES, this may decrease the autonomy in a society as a whole. Clinicians, driven by the inexorable logic of the ‘technological imperative’, may feel that they need to offer it. If PES becomes socially established, parents may feel compelled to make reproductive decisions that do not align with their values. For example, they may feel pressured to select against certain mental health conditions that they do not find harmful, or even that they consider part of the normal spectrum of human differences. (It is further worth noting that some of the same genes underlying some forms of psychiatric disorder tend to be associated with creativity and educational attainment.) These concerns may be exacerbated if parents start selecting for non-medical traits, such as height or intelligence, which could lead to a classic Red Queen effect – the perceived need to run faster and faster just to stay in place. Given the extreme lengths to which families will go to support their children’s college ambitions, it is not difficult to picture a similarly frantic race for advantage occurring 18 years earlier.
On the other hand, it is possible that PES will end up being used primarily by very specific patient populations. PES may be especially appealing to intended parents who have a previous child with an early life disease such as Type 1 diabetes, or who are affected themselves. Our research has shown that with PES the risk to future children of such couples could be substantially reduced, even in absolute terms. Many of the ethical, societal and practical problems with PES that we have described would become less worrisome in this setting, where utilisation is confined to limited populations. Additionally, it is probably unrealistic to worry that this procedure, even if applied population-wide, will meaningfully diminish overall genetic diversity, making the population more homogeneous, psychologically or otherwise. This is because polygenic traits and diseases are influenced by hundreds or even thousands of genes, such that the impact of PES on the frequency of any individual DNA variant in the population should be small.
However the use of the technology unfolds, it is crucial that the scientific debate remains evidence-based. The ability of PES to achieve some risk reduction seems guaranteed. But there is little clarity on exactly how much relevance the current genetic predictions have to babies to be born in the 2020s, given how future circumstances and treatments might affect risk. Moreover, the ability of intended parents to understand the procedure and the impacts of testing on wellbeing need to be evaluated. Regulation of the practice, whether by professional guidelines or by law, will be paramount for assuring the technology does not harm, impose on or mislead future patients.
It remains to be seen whether this form of embryo selection will end up being broadly socially accepted. We feel that there are still too many unknowns to state with confidence how the debate will, or should, play out. But based on what we have observed in the popular media, as well as in our scientific circles, there appears to be a strong reaction against the use of PES. Indeed, this topic may be one of the few that can unite Left and Right in a polarised society: many conservatives oppose ‘playing God’ and discarding embryos, while many progressives voice concern about the ableist implications of embryo selection.
It is important to remember, though, that many of the same arguments were made against IVF decades ago; a decade later against genetic screening of embryos for lethal diseases; and more recently against testing embryos for variants that increase breast cancer risk. Despite these arguments, these procedures are now widespread: approximately 2 per cent of births in the US derive from IVF, and genetic testing of any kind is performed in 45 per cent of IVF cycles.
Will PES, too, become accepted and widespread in the decades to come?