A mother in her mid-20s begins to have recurring thoughts of physically harming her baby. These thoughts make no sense to her. She deeply loves her baby, and thoughts of hurting him intentionally are immensely distressing to her, as they would be for any parent. She decides to take a shower while her baby sleeps. The shower has the desired effect of cleansing her of her disturbing thoughts. Gradually, her thoughts turn to more mundane matters.
But soon after she finishes showering, the thoughts of hurting her baby return, and they continue to do so, day after day. She becomes obsessed with the possibility that she might actually do harm to her child. Could she really do the things she’s imagining? The only time she’s free from these terrible thoughts is under the shower. She spends increasing periods each day showering, attempting to wash away her dreadful thoughts. Soon, she feels she must shower again to feel normal. She can see no other alternative.
Eventually, things get so bad she seeks medical help. She is diagnosed with obsessive compulsive disorder (OCD), and offered a combination of medication with psychotherapy. Neither of these treatments prove effective, so she is referred to the Amsterdam University Medical Center, and the psychiatrists on our team.
Our group specialises in deep brain stimulation (DBS), an innovative treatment in psychiatry offered to a small but significant number of patients who don’t respond to psychotherapy or medication. DBS involves the implantation of electrodes that deliver pulses of electrical stimulation to areas deep inside the brain.
We tell our new patient that DBS should have a significant chance of success where other treatments have failed, and she decides to give it a try. First, a team of neurosurgeons implant two electrodes deep inside her brain. She is given two weeks to recover from the surgery. Then a team of psychiatrists enter the scene, using a remote-control device to adjust the frequency, duration and amplitude of current from the electrodes to optimise the stimulation. Think of it as a kind of pacemaker for the brain.
At first, nothing changes, and our patient worries that she could be what we call a ‘non-responder’. Then we adjust the stimulation one more time, and she experiences something that literally astonishes her.
Up until this moment, she felt only the deep anxiety she has been struggling with every day, but an instant later she begins to feel good about her life. In a matter of seconds, the restrictions lift. She feels lighter, less burdened by her fear and anxiety. Her breathing slows, she feels more relaxed. Whereas before she felt completely dependent on the psychiatrists, she now feels able to relate to them as her equals. She is happier, and hopeful for her future.
Since 2005, our research group has treated 85 patients with OCD. As the trained philosophers on the team, our interest has naturally been piqued by the instantaneous changes in lived experiences we’ve observed in these patients. But we’re also puzzled: how could applying an electrical current to neuronal cells deep in the brain lead to such complex changes in the patient’s experience, like those we’ve just described? Why would electrically induced changes in the brain have an immediate impact on the suffering of patients for whom all other treatments in psychiatry have failed? If anxiety can be turned down in a split second, just by modifying the electrical activity of neurons, what does this tell us about the mind and its relation to the brain?
To learn more about how DBS has changed the lives of the patients we’re treating for OCD, we decided to carry out interviews with a group of them, eliciting responses that reflected as closely as possible these patients’ own personal stories of struggle and transformation after treatment with DBS. They told us that following DBS they felt more certain about themselves in their transactions with the world. They trusted in their own abilities for dealing with the world. Several patients told us they felt empowered by DBS:
DBS certainly has done something, because I am much stronger and powerful now. And much more like, you know, this is what I want, and this is what I will pursue, making my own choices. Before, I would never have done that, I didn’t dare.
Many patients told us they felt more assertive following their DBS treatment and were now able to make themselves more heard in social interactions:
Well, your mood improves, right, you become more cheerful – so yes, I started talking much more, I became much more assertive, I should say. I really stood up for myself much more, sometimes even a bit too much.
Interestingly, both in our clinical work and in these semi-structured interviews, patients often describe these kinds of changes as a feeling of increased self-confidence. This is interesting because self-confidence is not part of psychiatric assessment scales for OCD, and it wasn’t explicitly investigated in the semi-structured interviews we carried out.
Our patients experienced an expanded horizon of engagement and interest
Patients told us that they felt they could once again take part in ordinary mundane activities they had previously strenuously avoided because of their fears and anxieties. They could now shop for groceries, attend social gatherings, resume their hobbies and pursue old interests they had long since abandoned. They dared to do things they used to avoid. They were more open to possibilities, and once again able to think about, and make plans for, the future:
So then you see all these possibilities, and I have also started to look into things. And then I think: oh, I can do this, I can build that, and that’s actually not so hard … If it [DBS] had not been, then I maybe would not have even thought of doing something like that … But now I think: oh, I can give it a try, and if it doesn’t work out, that’s OK.
In sum, our patients experienced an expanded horizon of engagement and interest. Following DBS, they no longer confronted a world of threats and obstacles but were ready to engage with the possibilities on offer to them. Before DBS, a person with OCD would be rigid and restricted, compelled to act on their compulsions – all other alternative possibilities felt closed off. They experienced a lack of freedom. After DBS, patients tell us they again experienced a world of alluring, enticing and attractive possibilities. For instance, a patient might see the prospect of sailing a boat they own as an attractive possibility once again.
There are two sides to the increased self-confidence we see in our DBS patients, corresponding to the self and the world. On the side of the world is the expanded range of possibilities that the patient is now open to engaging with – activities previously deemed impossible. On the side of the self, new ways of being are now available – for example, the possibility of becoming a skipper and sailing around Europe. Our patients literally relate to their own existence in a new, more open way, with greater understanding of who they fundamentally are. When someone is entranced, once more, by exploring the waterways of Europe, they’re seeing an entirely new way to live as possible.
In his magnum opus Being and Time (1927), Martin Heidegger used the notion of ‘projection’ (Entwurf) to describe the two dimensions to self-confidence we distinguished in patients receiving DBS. In ordinary German usage, the noun Entwurf and the verb entwerfen refer to the sketching of some project to be carried out (for instance, an architect drawing a new building in a sketchbook). Heidegger points out that projection is not a matter of thinking up and carrying out a plan. Instead, it refers to the freedom a person has to press forward into a range of possibilities; it means taking a stand on who we are. With Entwurf, Heidegger hoped to capture a forward momentum to the living of life.
Human beings can seize hold of possibilities and embark on projects that shape their self-understanding – the person’s understanding of who they are. For Heidegger, a person’s self-understanding of who they are comes from an openness to the world and its possibilities. Yet for the person with OCD, the world is permeated by an atmosphere of compulsivity. Therefore, that person’s openness to the world shrinks to the possibilities they feel compelled to act on. Before her treatment, the young mother who came to our clinic felt she had no recourse but to shower for even a temporary sense of normality. The range of possibilities she saw was severely restricted by her anxiety. This meant that her options in life were restricted too. Following DBS, the range of inviting possibilities she saw expanded, and with it her self-understanding and self-confidence, much like a flower bud that opened up when its season came. Her increased openness to the world allowed her to grow and flourish as a person once more.
The growth in self-confidence brings the patient to a place where they can begin to respond to psychotherapy
The increased self-confidence the patient experiences with DBS can be understood using Heidegger’s concept of projection – the ability to press ahead into a range of possibilities that contribute to self-understanding. Heidegger felt it was the core of being human to care about such possibilities, but OCD interferes. The self-understanding of the person with OCD is severely hampered by their inability to press forward into the inviting possibilities that matter to them. DBS helps restore the possibility to shape who they are through their actions.
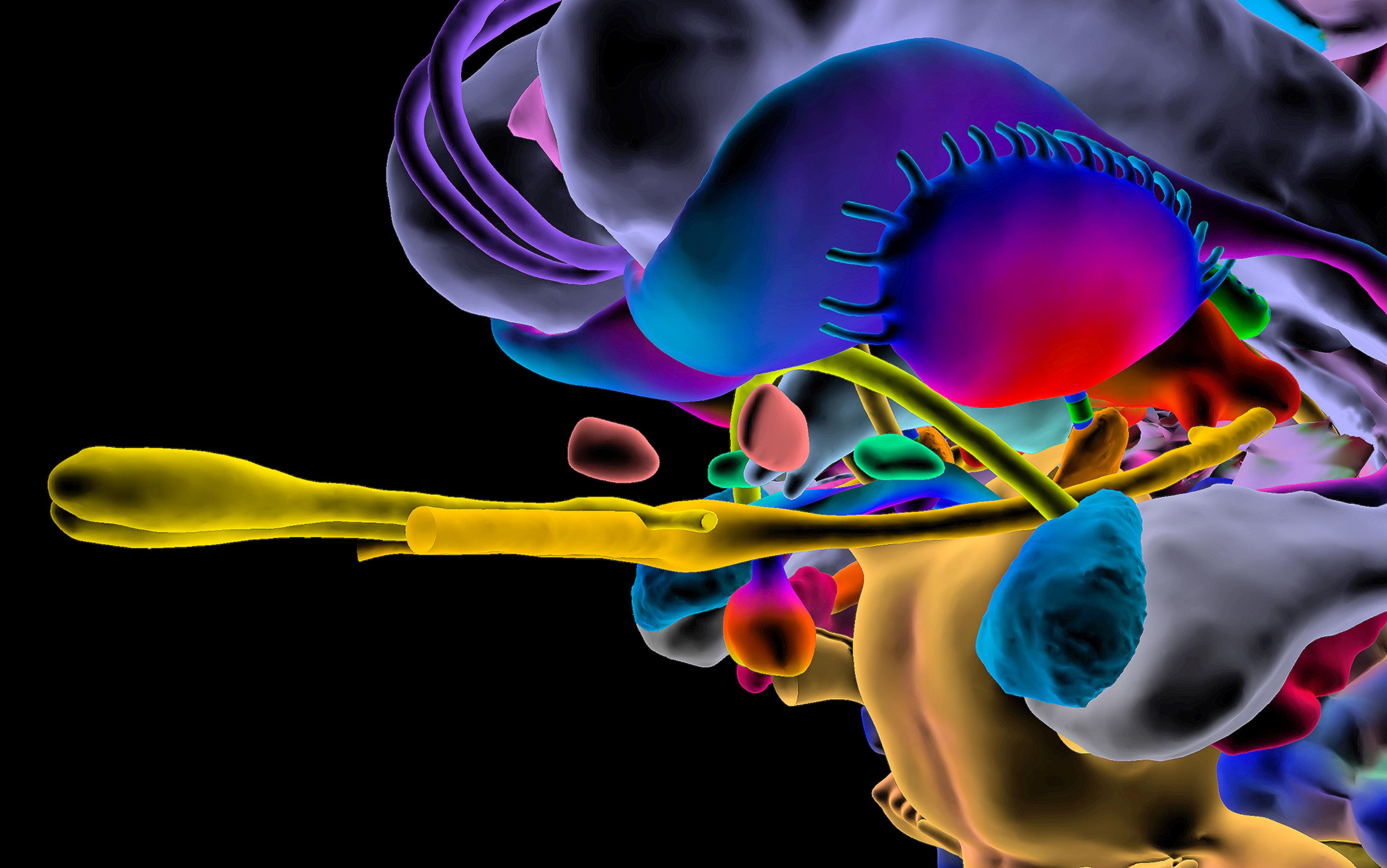
Why does electrical stimulation of the brain restore the ability to project a possible future not determined by a patient’s illness? Direct impact on brain function and neuronal mechanisms might provide an answer. The patients being treated in our hospital, for instance, receive stimulation of brain areas located in the ventral striatum, leading to changes in the large-scale connections that form between the striatum, the prefrontal cortex and the amygdala, brain areas that play a role in decision-making, memory and thinking. One might hypothesise that the transformation following DBS can be explained by changes to this once-dysfunctional neural network.
But this cannot be the whole answer. The changes the patient experiences following DBS go far beyond a decrease in their obsessions and compulsions. They include a wholesale change in the person, including an increase in self-confidence; yet loss of self-confidence is not among the symptoms currently used to diagnose OCD.
The reduction in symptoms that patients experience following DBS are perhaps better thought of in the context of the growth in self-confidence, and the effect this has on the patient’s life as a whole. For example, several OCD patients in our study noted that their attitude towards their compulsions had become quite different following their treatment with DBS: they were no longer so troubled by them. Perhaps the growth in self-confidence brings the patient to a place where they can begin to respond to psychotherapy that can help them make further progress in reducing their obsessions and compulsions.
We have now come full-circle in our effort to puzzle out the DBS effect: why, exactly, is DBS so transformative – not just eliminating OCD symptoms, but increasing self-confidence and openness to the world? And how can we make sense of self-confidence in the context of electrically induced changes in the brain? It could be that changes in the brain and an increase in self-confidence are both needed to set the sick person right. Understanding the effects of DBS on the brain might therefore be only a part of the explanation of how DBS changes the person.
It is the whole person who responds to DBS, and not only the parts of their brain where the electrodes are implanted. DBS changes many aspects of how a person engages with the world. Their social interactions, tendency to reflect and ruminate, mood, interests and, more generally, their self-confidence in life. Even for those without a pathology, the experience of over- and under-confidence can be common throughout life. Think of going into an interview where your dream job is at stake. In this kind of situation, many might experience a lack of self-confidence. Overconfidence on the job, on the other hand, can lead to precipitous calculations and risks. Too much self-confidence can tip over into impulsive acts that appear pathological; too little self-confidence can lead to anxiety and lack of trust in oneself and the world.
Why might self-confidence prove crucial to recovery from OCD? The answer lies in Heidegger’s notion of projection, which might exist along a continuum with normal everyday anxiety and uncertainty at one end and pathologies such as OCD at the other. Disturbances in projection could be a risk factor for mental illness missed by psychiatry until now. Projection can also provide a bridge from illness back to being well. DBS patients experience an expanded horizon of engagement and interest. They feel empowered to once again take up possibilities that are important to them. Perhaps it is projection (the person’s expanded openness to the world) that inspires self-confidence, providing a path from illness to health.
The world of the young mother who came to our clinic had shrunk to the four walls of her house and caring for her child. As OCD took hold of her, her world shrank further, and so did her self-understanding. Her life was consumed by the rituals she developed to offer relief from her distressing thoughts. Her unwanted thoughts about physically harming her child took on a life of their own. All of us experience unwanted, socially inappropriate thoughts from time to time. We might even find ourselves surprised and disturbed by these thoughts. Mostly, we somehow avoid getting too caught up in such thoughts. We have a basic trust in ourselves and the world. However, as her OCD took hold, the young mother began to doubt herself, and what she might do. Her showering routine was her way of compensating for this uncertainty. The predictability of her cleansing ritual provided temporary relief from her uncertainty.
Most of us would approach El Capitan with fear. Honnold approaches it with a desire to learn and grow
By contrast, the self-confident person trusts in themselves and the world. They’re open to the possibilities the world has to offer. Consider as an example Alex Honnold, a master of ‘free solo climbing’: he slowly but surely ascends the world’s biggest cliff rockfaces without any ropes, harnesses or protective equipment. In 2017, he achieved his dream of climbing the 3,000-foot El Capitan in Yosemite National Park without any support.
A documentary crew accompanied him over the long period of preparing for the climb, trying, failing and eventually succeeding. In the subsequent film Free Solo (2018), Honnold shows how his experience of climbing is one of slowly, calmly and confidently exploring the rockface. Most of us would approach El Capitan with fear. Honnold approaches the climb with a desire to learn and grow through mastering this challenge. Through his meticulous preparation, he has trained himself to be fearless, and to be tolerant of the intense stress elicited by life-and-death situations. A climb that would strike even the most skilled free solo climbers as impossible is a possibility he was able to playfully explore, and eventually master.
Sensation-seeking behaviours such as free solo climbing might strike the risk-averse among us as an unhealthy personality trait. Why is Honnold’s free soloing not an example of extreme impulsivity and risk-taking? His self-confidence is different from the overconfidence of individuals who experience pleasure from taking risks. For Honnold, the thrill of the climb doesn’t seem to come from living life on the edge, risking his life in the process. His calm confidence allows him to explore climbing possibilities at the edge of his own abilities. This openness to possibility allows him to learn and grow in his skill. In short, self-confidence provides him with possibilities to fulfil his potential as a climber, to flourish in an activity to which he’s dedicated his life.
Honnold’s story offers an important clue as to why self-confidence might prove to be important for a person’s mental health. Self-confidence can be understood as a person’s openness to the world and the possibilities it offers. So long as the person is ill with OCD, they will remain closed to the world. They will doubt themselves and the world, where others would feel unworried and move ahead. Their response to this doubt is to retreat from the world into the carefully staged rituals that allow them to manage their uncertainty. Honnold has also trained himself to manage his stress and fears. However, he differs from people living with OCD insofar as he’s now able to use his high tolerance for stress to explore the very edge of what’s possible in the world of free solo climbing. Self-confidence can open the door to mental health because the self-confident person is open to the world and its possibilities. This openness is what allows the person to find their way to lead a fulfilling life of their own design.
The authors gratefully acknowledge support from the European Research Council (ERC Starting Grant number 679190 awarded to Erik Rietveld) and to Amsterdam Brain and Cognition for a research grant (awarded to Damiaan Denys and Erik Rietveld).
To read more on mental health, visit Psyche, a digital magazine from Aeon that illuminates the human condition through psychology, philosophical understanding and the arts.