When Ronald Ross tipped over the water tank outside his bungalow in Bangalore, it began a lifelong battle against mosquitoes. It was 1883 and Ross, only two years out of medical school, was the British Army’s new garrison surgeon. Overall, he was happy with the posting – he considered the city, with its sun, gardens and villas, to be the best in southern India.
He was less enthusiastic about the mosquitoes. Having arrived to find his room filled with the sound of buzzing wings, he decided to hunt down and destroy their breeding ground in pools of stagnant tank water. The ploy worked: as he drained the tanks, mosquito numbers fell.
The longer Ross spent in the region, the more he began to suspect that those mosquitoes transmitted malaria, an often-lethal disease with spiking fevers and other symptoms resembling a devastating flu. The disease had probably been around since Homo sapiens first evolved. Its name came from Renaissance Italy; ‘mala aria’, or ‘bad air’, referred to the suspected cause of the disease.
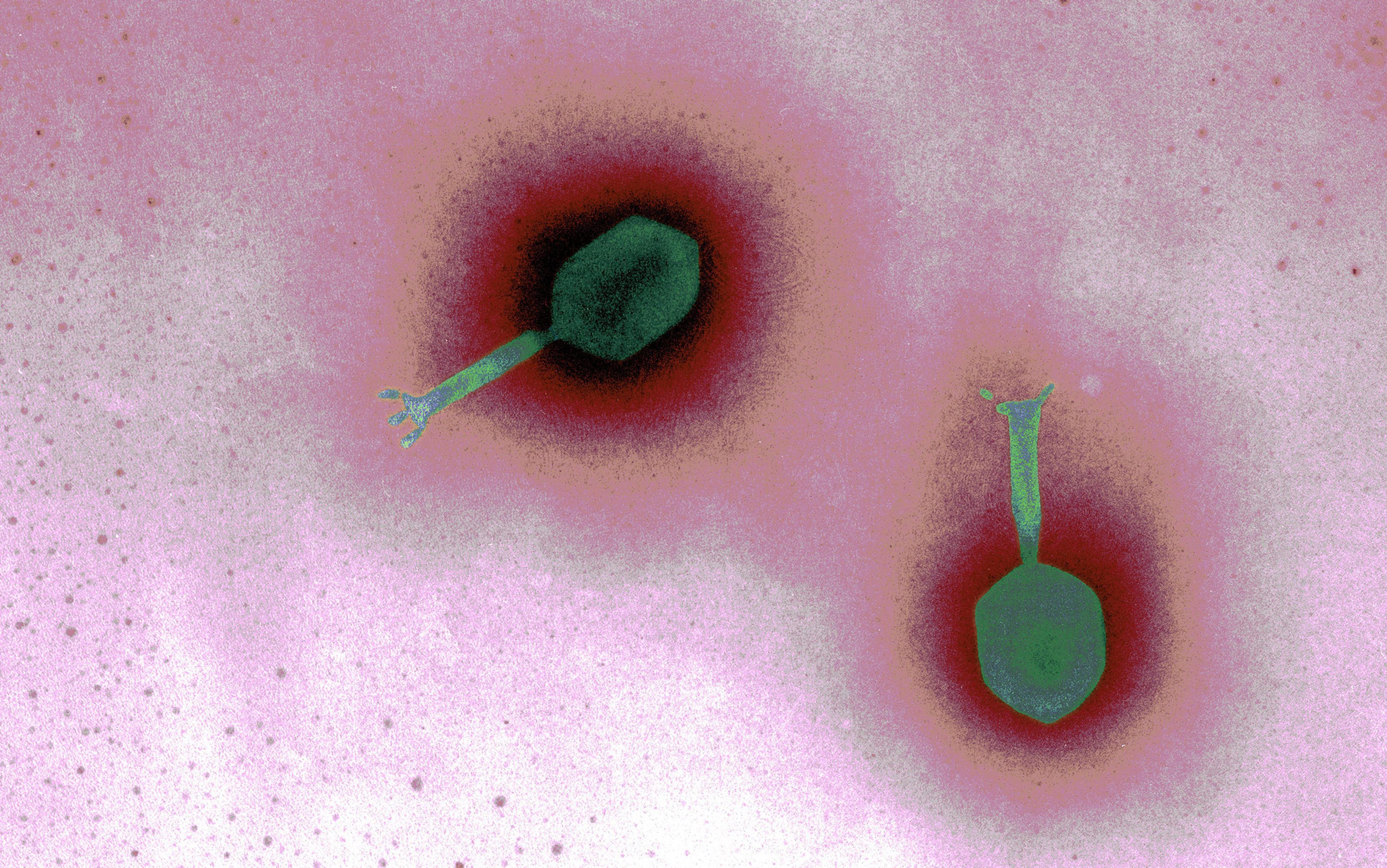
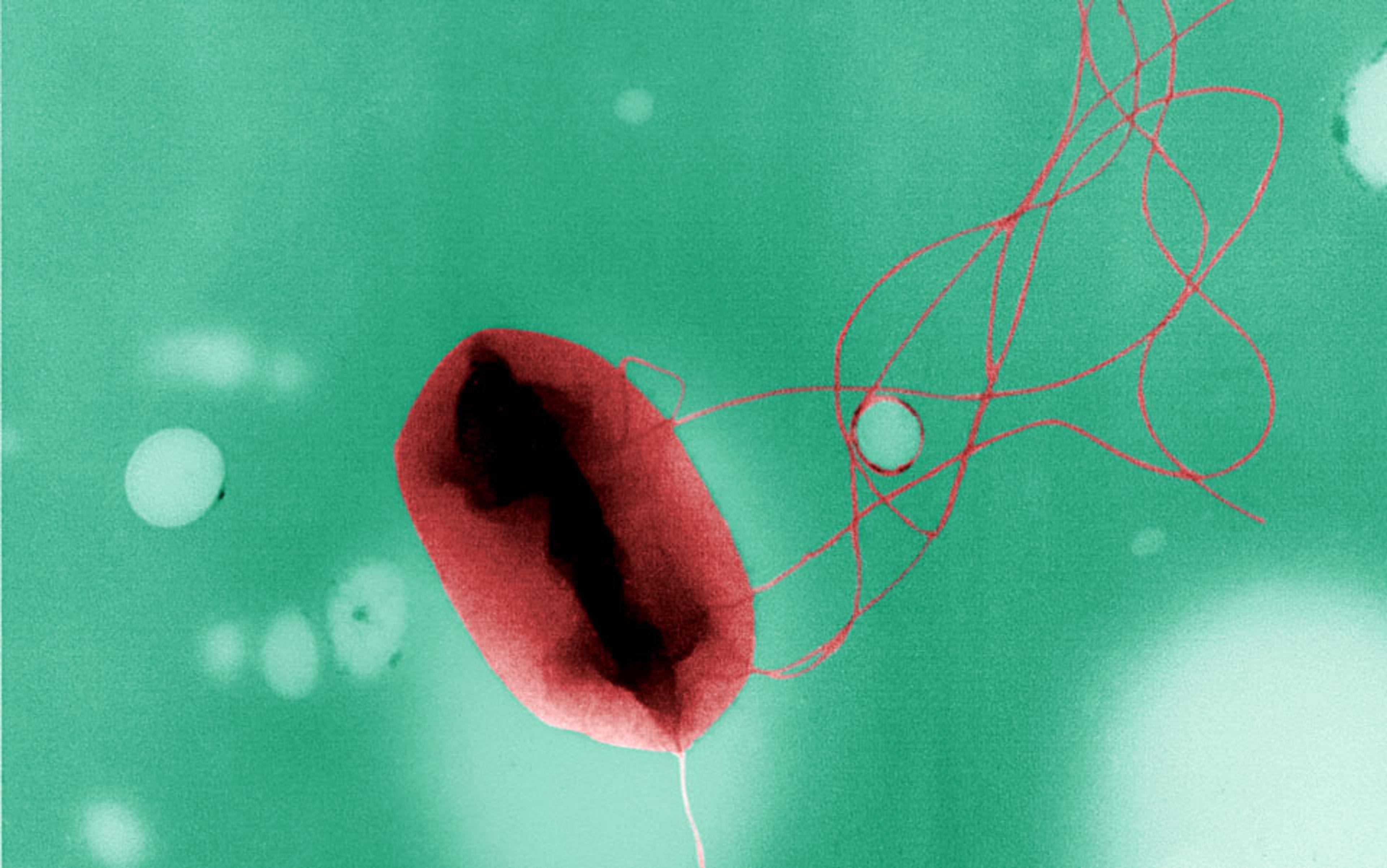
To prove the connection between mosquitos and malaria, Ross experimented with birds. He allowed mosquitoes to feed on the blood of an infected bird then bite healthy ones. Not long afterwards, the healthy birds came down with the disease, too. To verify his theory, Ross dissected the infected mosquitoes, and found malaria parasites in their saliva glands. Those parasites turned out to be Plasmodium, identified by a French military doctor who had discovered the bug in the blood cells of infected patients just a few years before.
Next, Ross wanted to show how the disease could be stopped, and his experiment with the water tank pointed the way. Get rid of enough insects, he reasoned, and malaria would cease to spread. To prove his theory, Ross, a keen amateur mathematician, constructed a theoretical model – a ‘mosquito theorem’ – outlining how mosquitoes might spread malaria in a human population. He split people into two groups – healthy or infected – and wrote down a set of equations to describe how mosquito numbers would affect the level of infection in each.
The human and mosquito populations formed a cycle of interactions: the rate at which people got infected depended on the number of times they were bitten by infected mosquitos, which depended on how many such mosquitos there were, which depended on how many humans had the parasite to pass back to those mosquitos, and so on. Ross found that for the disease to simmer along steadily in a population, as it did in India, the number of new infections per month would need to be equal to the number of people recovering from the disease.
Using his model, Ross showed that it wasn’t necessary to remove every mosquito to bring the disease under control. Destroy enough mosquitoes, and people infected with the parasite would recover before they were bitten enough times for the infection to continue at the same level. Therefore, over time, the disease would fall into decline. In other words, the infection had a threshold, with outbreaks on one side and elimination on the other.
Ross’s work, which won him a Nobel Prize in 1902 and a knighthood in 1911, set the stage for a new mathematical way of thinking about disease outbreaks from bubonic plague to influenza. His insight influenced vaccine policy through the concept of ‘herd immunity’: vaccinate a sufficient proportion of the population, and the disease will fail to take off. It means that vaccination can work even if a few people are left unprotected. Although the specific control measure is different – giving vaccines rather than removing mosquitoes – the principle is the same. As long as we remove enough links in the chain of events that generate infections, the disease will die out. It isn’t necessary to vaccinate everyone, or remove every mosquito; if we reach the critical threshold, the infection will struggle to cause outbreaks in the population.
Other researchers had studied infections in a mathematical way before Ronald Ross, but their approaches focused on past events. Take the physician John Snow, who had used logical reasoning to trace the cause of the 1854 London cholera outbreak. As with malaria, most people at the time blamed cholera on ‘bad air’. But when Snow plotted the locations of all disease cases on a map, he noticed that the water pump on Broad Street in Soho was the local water source for infected households. He reasoned that patients were catching cholera from contaminated water, which meant that removing the source on Broad Street would halt the spread.
Rather than look backwards, Ross looked ahead, and his enthusiasm for predicting the future convinced colleagues to join in. One was a young Scotsman named Anderson McKendrick, a mathematician and member of the Indian Medical Service whom Ross had met during an anti-malarial campaign in Sierra Leone. McKendrick came down with a tropical gut disease in 1920 and, like Ross before him, ultimately left India. Back in Edinburgh, he took a position as superintendent of the Laboratory of the Royal College of Physicians. It was there that he met William Kermack, a junior chemist who also had an interest in infectious diseases.
Together, the pair extended Ross’s method of examining the interactions that drive epidemics. Along with looking at infections that simmered away over time, such as malaria, McKendrick and Kermack studied diseases such as the plague, which exploded through a population before disappearing again.
From influenza to plague, the number of cases in a real epidemic often rises exponentially at first
Like Ross, they grouped the hypothetical population into groups that were healthy or infected. But this time there were no mosquitoes: the infection spread directly from person to person. As before, individuals started out susceptible to infection. Upon exposure, they would move into the infectious group. Finally, they would leave the infectious group, either because they’d gained immunity to the disease (a reasonable assumption for infections such as measles and pandemic flu) or because they had died (as was common with plague).
Progress was not always smooth. In 1924, Kermack was blinded in a lab accident, so from that point onwards he did all his calculations in his head. He and McKendrick eventually published their findings in 1927, in a paper titled ‘A Contribution to the Mathematical Theory of Epidemics’ in the Proceedings of the Royal Society of London. Over the course of 20 pages, they tackled one of the most important questions in epidemiology: what causes an epidemic to end?
From influenza to plague, the number of cases in a real epidemic often rises exponentially at first. After a while, the disease reaches a peak level, and then the number of new cases starts to decrease. When McKendrick and Kermack began their research, people generally gave two possible reasons for the decline. Either the epidemic faded away because the infection had become less potent over time, or because there were no susceptible people left – everyone had been infected and either died or become immune.
In their model, McKendrick and Kermack assumed that the pathogen stayed the same throughout the epidemic; the infection did not weaken over time. And yet the model still produced an eventual decline in cases. When the pair compared the model to the 1905 outbreak of plague in Bombay, the predicted number of cases matched the real disease level.
So was the decrease in infection caused by a lack of susceptible people? Apparently not: in the model, there were always some susceptible individuals remaining at the end of the outbreak. McKendrick and Kermack had demonstrated that epidemics don’t necessarily decline because everyone has been infected. They can also end because there aren’t enough infected people left to sustain transmission. Once enough people are immune, infected individuals are unlikely to meet another susceptible person, which means that they generally recover before infecting others.
Measles is at the wildfire end of the scale. In an unvaccinated population, it has a reproduction number between 12 and 18, explaining why it has always been a childhood disease
This effect is inevitable in the later stages of an outbreak, but it is also possible to force an epidemic into this situation. In Ross’s model, the reduction in infection came from getting rid of mosquitoes. During a vaccination campaign, it comes from targeting a large chunk of the susceptible population.
It would be decades before the next major breakthrough in the theory of epidemics. In the 1970s, mathematician Klaus Dietz and the ecologists Roy Anderson and Robert May began their pioneering work on the idea of ‘the reproduction number’: the average number of people a typical infectious case will pass the disease onto. The reproduction number is useful because it captures all the processes that influence transmission, from social behaviour to severity of infection, into a single measurement. The size of this number can reveal what will happen during an outbreak. If the reproduction number is less than 1, each case will on average produce less than one additional infection, and the infection will fade away without causing a large outbreak. If it is greater than 1, then we would expect the number of cases to grow over time as the infection spreads through a population.
There are several ways to estimate the reproduction number of an infection. If we know how long people are infectious for – and hence the average time between each ‘generation’ of disease cases – we can estimate the reproduction number by looking at how quickly the epidemic grows. Alternatively, we can estimate it by calculating the average age at which people experience their first infection. The more infectious a disease is, the sooner a person will become infected.
By calculating reproduction numbers, we can quantify and compare different infections. Measles is at the wildfire end of the scale. In an unvaccinated population, it has a reproduction number that lies somewhere between 12 and 18. This explains why measles has always been a childhood disease; a high reproduction number drives down the average age of infection. In contrast, the 1918 pandemic influenza strain – the infamous ‘Spanish flu’ – had a reproduction number of around 2 or 3. Because the disease came with a high fatality rate, even this relatively low reproduction number was enough to create widespread devastation. In the middle, we have infections such as polio (5 to 7) and mumps (4 to 7).
Although the reproduction number does not tell us how fast an infection will spread from person to person, it does show how much effort is required to eradicate a disease through vaccination. For a disease such as measles, we need to vaccinate a lot of the population to reduce the average number of secondary cases, and hence get the reproduction number below that crucial value of 1. But the reproduction number isn’t just useful for studying familiar infections. It can also help us deal with new disease threats.
On 21 February 2003, a man checked into room 911 of Hong Kong’s Metropole Hotel. He did not feel well. He was in the city for his nephew’s wedding, and had started to come down with something on the trip over from southern China. Within 24 hours, he was gravely ill in an intensive care unit, and in 10 days he was dead.
The infection was dubbed Severe Acute Respiratory Syndrome (SARS) and, before long, cases started appearing in other cities too: Singapore, Bangkok, even Toronto. During this period, there were several things that health agencies needed to find out: how transmissible was the virus; who had the infected come into contact with; and which measures were proving most effective in keeping infection rate down?
During the spring of 2003, researchers at Imperial College London used mathematical models to examine SARS data from Hong Kong. They found that when no control measures were in place – such as at the start of the outbreak – SARS had a reproduction number of 2 to 3.
When vaccinating against an infection with a reproduction number of 3, at least two-thirds of the population need to get jabs to control the outbreak. This way, less than a third of the population will be left susceptible. Hence each infectious person will generate less than one additional case on average, sending the disease into decline.
This approach works for infections such as measles, but unfortunately there wasn’t a vaccine for SARS when it first appeared. The same problem exists for most new infections, from Middle East Respiratory Syndrome (MERS) to Ebola. Making a vaccine takes time, especially when it is for a virus nobody has seen before. During the SARS epidemic, researchers therefore had to think beyond simple vaccination thresholds.
If there is no effective vaccine or treatment for an infection, health agencies have two basic options to reduce the spread of infection: make sure people with disease symptoms are properly isolated, and trace the people with whom patients have recently come into contact so they can be tested for the disease.
During the SARS outbreak, many infected people reduced their movements and social interactions, helping to bring the epidemic under control.
Analysing the SARS outbreak using mathematical models, the researchers found that isolating patients had proven very effective in controlling in the infection. Many infected people reduced their movements and social interactions too, which also helped to bring the epidemic under control.
The World Health Organization declared the SARS epidemic to be under control on 5 July 2003. But the Imperial College researchers still wanted to know why isolation had been so successful and whether it would work for other infections too. The group developed a mathematical model to see how much isolating patients affected disease transmission, and found that the effectiveness depended not just on the reproduction number but also on the proportion of infections that occur before symptoms appear.
During the SARS outbreak, people were most infectious after they became visibly ill. This is why isolation was effective: once people with symptoms were contained, there were very few opportunities for infection. The situation is very different for influenza, where people without symptoms are responsible for a large chunk of infections. In a flu outbreak, isolation and quarantine will be less effective because there is a good chance the patient will have infected others before they became ill.
In the century since Ross published his mosquito theorem, such analysis has become increasingly common in the study and management of epidemics. When faced with new infections – such as the current outbreak of Ebola in West Africa – we can use mathematical models to estimate whether the reproduction number is near to that crucial value of 1; so far there’s evidence that Ebola’s reproduction number could be as high as 2 in some areas, which is why cases are still increasing exponentially.
By viewing epidemics as a dynamic process, we can also evaluate potential control measures. Over the next few winters, the UK will introduce influenza vaccination for all children based in part on new mathematical models. Researchers looked at what effect vaccinating different combinations of age groups could have, and what would happen if only a certain percentage were vaccinated. The results suggested that targeting children and older adults would be the best way to reduce influenza illness and death.
The ability to make predictions about epidemics is one of the major strengths of mathematical approaches. Using models, we test control strategies without interfering with the real world. We can therefore compare treatments and interventions before putting them into practice.
Thanks to Ross and his successors, we no longer have to tip over the water tank to find out what effect it might have.