The latest epidemic to terrify the Western world is Ebola, a virus that has killed hundreds in Africa in 2014 alone. No wonder there was so much worry when two infected health care workers from the United States were transported home from Liberia for treatment – why bring this plague to the US, exposing the rest of the country as well? But the truth is that Ebola, murderous though it is, doesn’t have what it takes to produce a pandemic, a worldwide outbreak of infectious disease. It spreads only through intimate contact with infected body fluids; to avoid Ebola, just refrain from touching sweat, blood or the bodies of the sick or dead.
Yet no logic can quell our pandemic paranoia, which first infected the zeitgeist with the publication of Laurie Garrett’s The Coming Plague (1994) and Richard Preston’s Hot Zone (1995). These books suggested that human incursion into rainforests and jungles would stir deadly viruses in wait; perturb nature and she nails you in the end. By the late 1990s, we were deep into the biological weapons scare, pumping billions of dollars in worldwide government funding to fight evil, lab-made disease. As if this weren’t enough, the panic caused from 2004 to 2007 by reports of the H5N1 or bird flu virus etched the prospect of a cross-species Andromeda strain in the Western mind.
The fear seems confirmed by historical memory: after all, plagues have killed a lot of people, and deadly diseases litter history like black confetti. The Antonine Plague, attributed to measles or smallpox in the year 165 CE, killed the Roman Emperor Marcus Aurelius and millions of his subjects. The Justinian Plague, caused by the deadly bacterial pathogen Yersinia pestis, spread from North Africa across the Mediterranean Sea to Constantinople and other cities along the Mediterranean. By 542, infected rats and fleas had carried the infection as far north as Rennes in France and into the heart of Germany. Millions died.
Then there was the Black Death of 1348-50, also caused by Yersinia pestis, but this time spread by human fleas and from human lung to human lung, through the air. The plague spread along the Silk Road to what is now Afghanistan, India, Persia, Constantinople, and thence across the Mediterranean to Italy and the rest of Europe, killing tens of millions worldwide. Of all the past pandemics, the 1918 influenza (also known as the Spanish flu) is now considered the über-threat, the rod by which all other pandemics are measured. It killed 40 million people around the globe.
It was the great Australian virologist Frank Macfarlane Burnet who argued that the deadliest diseases were those newly introduced into the human species. It seemed to make sense: the parasite that kills its host is a dead parasite since, without the host, the germ has no way to survive and spread. According to this argument, new germs that erupt into our species will be potential triggers for pandemics, while germs that have a long history in a host species will have evolved to be relatively benign.
Many health experts take the notion further, contending that any coming plague will come from human intrusion into the natural world. One risk, they suggest, comes when hungry people in Africa and elsewhere forge deep into forests and jungles to hunt ‘bushmeat’ – rodents, rabbits, monkeys, apes – with exposure to dangerous pathogens the unhappy result. Those pathogens move silently among wild animals, but can also explode with terrifying ferocity among people when humans venture where they shouldn’t. According to the same line of thought, another proposed risk would result when birds spread a new pandemic strain to chickens in factory farms and, ultimately, to us.
But there’s something in these scenarios that’s not entirely logical. There is nothing new in the intimate contact between animals and people. Our hominid ancestors lived on wildlife before we ever evolved into Homo sapiens: that’s why anthropologists call them hunter-gatherers, a term that still applies to some modern peoples, including bushmeat hunters in West Africa. After domesticating animals, we lived close beside them, keeping cows, pigs and chickens in farmyards and even within households for thousands of years. Pandemics arise out of more than mere contact between human beings and animals: from an evolutionary point of view, there is a missing step between animal pathogen and human pandemic that’s been almost completely overlooked in these terrifying but entirely speculative ideas.
According to the evolutionary epidemiologist Paul W Ewald of the University of Louisville, the most dangerous infectious diseases are almost always not animal diseases freshly broken into the human species, but diseases adapted to humanity over time: smallpox, malaria, tuberculosis, leprosy, typhus, yellow fever, polio. In order to adapt to the human species, a germ needs to cycle among people – from person to person to person. In each iteration, the strains best adapted to transmission will be the ones that spread. So natural selection will push circulating strains towards more and more effective transmission, and therefore towards increasing adaptation to human hosts. This process necessarily takes place among people.
A pathogen must force its new human host to act as a germ dispensary system: sneezing, coughing, spewing germ-laden particles in the air
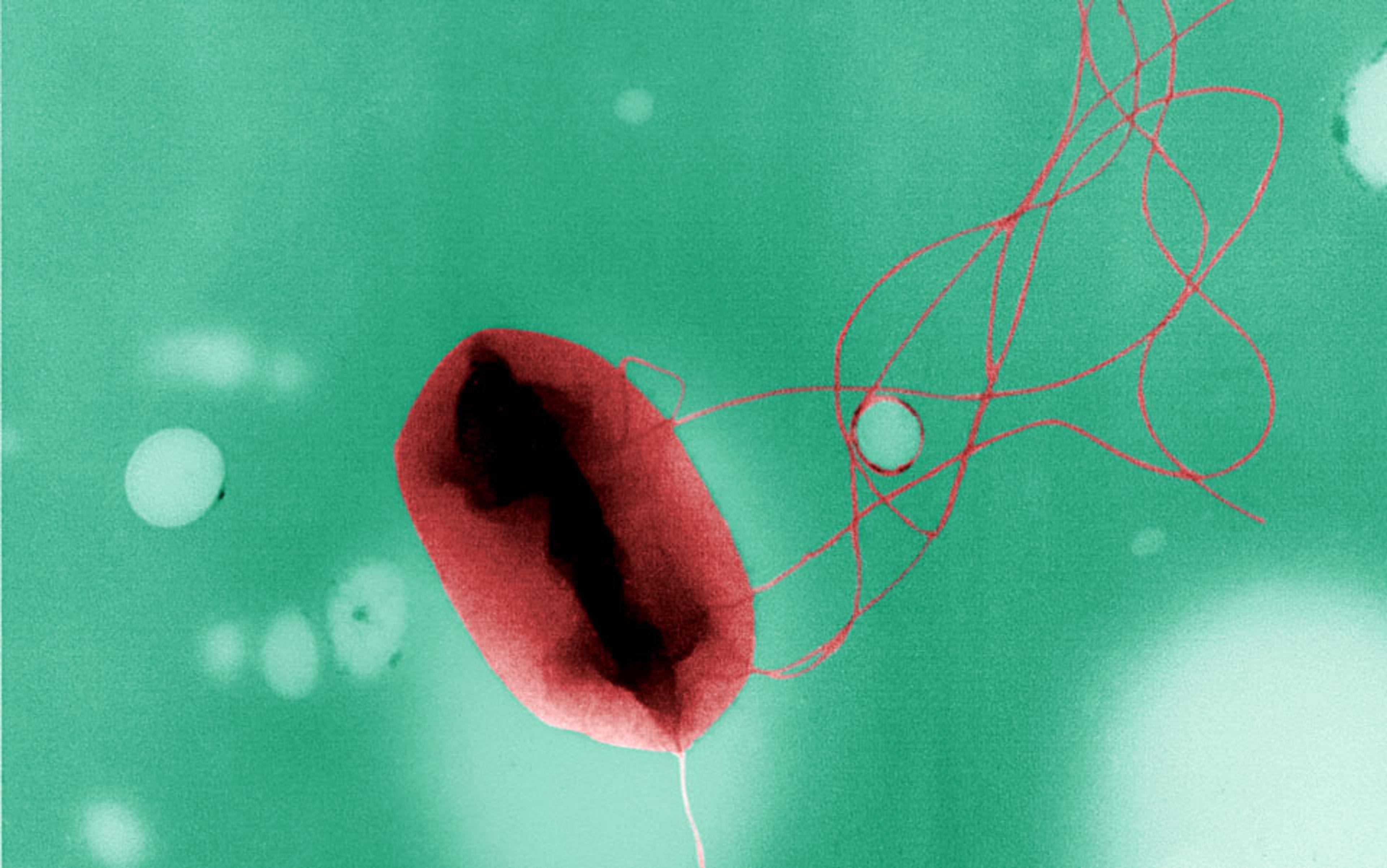
That is why the idea that highly pathogenic animal viruses such as H5N1 bird flu cycling among chickens, for example, can suddenly mutate into a lethal, transmissible human virus makes little evolutionary sense. Adaptation to a new host is a precise and delicate business. To be a human-adapted germ means having the ability to infect human cells, to overcome human immunity, and to manipulate the human host into shedding the germ.
A pathogen must force its new human host to act as a germ dispensary system: sneezing, coughing, spewing germ-laden particles in the air, or passing them through diarrhoea. To make us sneeze, a cold or flu virus somehow piggybacks on our evolved tendency to sneeze and cough to rid ourselves of irritants, whether that’s pollen or virus. Sneezing out virus might help you reduce your viral load and recover more quickly, but it also ensures that your co-workers go home with a dose of what ails you. A virus that does not cause symptoms is much less likely to transmit. On the other hand, if you are flattened immediately, the pathogen could be too virulent, immobilising you so thoroughly that you can’t get out to spread the disease. (Ebola is a standout example here.)
But once they evolve the knack for human-to-human transmission, these same killer pathogens can cause devastating human disease. The usual suspects are well-known: smallpox, which survives in the external environment; cholera, which spreads in water; malaria, carried by insects; and Staphylococcus aureus, spread by unwitting hospital attendants and known today in deadliest, most antibiotic-resistant form as MRSA.
One mysterious ancient outbreak, the Great Plague of Athens, shows how deadly epidemics unroll in time. The Plague – said to have been caused by typhus, measles, small pox or Ebola, depending on whom you ask – exploded in Athens in the summer of 430 BCE, during the early days of the Peloponnesian War, a 27-year struggle between Athens and Sparta over hegemony in the Hellenic world. Pericles, the de facto leader of Athens, who pushed for war, developed a defensive strategy that proved fatal, to him and to as many as a third of Athenian citizens. He insisted on bringing all citizens – people who lived in the towns and rural areas outside the walled city – into Athens, leaving the rest of the city-state to be ravaged by the invading Spartans. The Athenian Long Walls ran down to the separate ports of Piraeus and Phaleron, each of which lay about four miles from the City of Athens proper. Thus sealed off, fronting only on the sea, Athenians could shelter safely, Pericles argued, until the Peloponnesian War was won.
The normal population of the city was around 150,000. Scholars estimate that 200,000 to 250,000 farmers and townsmen and their families came streaming in, bringing everything they could carry with them – down to the woodwork on their farmhouse walls. But Pericles had made no provision for the newcomers, who were used to their country manors, their quiet towns, their open fields. A few had homes or relatives within the walls. But most had nowhere to go, and huddled in stifling huts, or in tents flung up in the narrow spaces between the walls. The crowded encampments were ripe for virulent infection.
Physicians and attendants died quickly, and the only people who could care for the sick were survivors immune to further infection
That infection came from the sea, the portal that Pericles had left open to feed the Athenian people and bring in enough money to keep the war effort alive. The Athenian historian Thucydides tells us that the disease originated in Ethiopia, travelled northward into Egypt and Libya, moved across the Mediterranean to the island of Lemnos, and on to Athens. ‘There was no record of the disease being so virulent anywhere else or causing so many deaths at it did in Athens,’ wrote Thucydides, and we have no reason to doubt him. This is a critical bit of information. It tells us that the Great Plague evolved: it became much more lethal in the great refugee camp that wartime Athens had become. Thucydides continued:
People in perfect health suddenly began to have burning feelings in the head; their eyes became red and inflamed; inside their mouths there was bleeding from the throat and tongue, and the breath became unnatural and unpleasant. The next symptoms were sneezing and hoarseness of voice, and before long the pain settled on the chest and was accompanied by coughing. Next the stomach was affected with stomach-aches and with vomitings of every kind of bile that has been given a name by the medical profession, and this being accompanied by great pain and difficulty. In most cases there were attacks of ineffectual retching, producing violent spasms; this sometimes ended with this stage of the disease, but sometimes continued long afterward.
Thucydides goes on to describe rashes, delirium, mental confusion and, among the survivors, blackened, dead tissue on the extremities, and sometimes blindness. This was a highly virulent, transmissible, systemic disease. Physicians and attendants died quickly, and the only people who could care for the sick were survivors immune to further infection.
The Athenian plague shows how a disease of mild to moderate virulence can heat up in what we can only call a ‘disease factory’ – a place where the sick are trapped together with the well, causing infection to spread like wildfire. If the Athenian infection was typhus, the most likely culprit, it would normally be spread by the human body louse and its infected faeces. There must have been body lice among the Athenian squatters. Usually just scratching lice bites, thus digging louse faeces inadvertently into the skin, causes transmission. But in crowded conditions, transmission of typhus can be more direct. For instance, in the Serbian prison camps of the First World War, where typhus was rampant, transmission through the air – possibly caused by aerosolised louse faeces – was known to occur. The right conditions, in other words, can cause the short-term evolution of a louse-borne disease into something explosive.
As Ewald has shown, a similar evolutionary process gave rise to the 1918 flu, propelled by the trench-warfare system of the Western Front. In the spring of 1918, a first wave of mild flu broke out in the US, and spread across the country to the troop ships loading for Europe. From those ships, the infection spread into the trenches, where it swiftly heated up to deadly virulence in the disease factory conditions of the Front: the trenches, the trains, the trucks moving the wounded and the sick together, where virus from people immobilised by illness was able, over and over, to infect the well. The whole system was a giant viral delivery service. The disease left the Western Front by several ports and exploded across the planet, killing about 2.5 per cent of those it infected – and it infected hundreds of millions.
This predatory influenza was not caused by some random combination of bird flu genes, as the new plague paranoia predicts. Both the Athenian Plague and the 1918 flu evolved in predictable Darwinian fashion. Germs that ravage the body more swiftly and effectively will outcompete milder strains. If those lethal strains have repeated access to fresh hosts, the brakes on virulence are off, and deadly disease evolves and spreads.
Looking at epidemics and pandemics through this evolutionary lens makes it clear that the most important condition necessary for the evolution of virulent, transmissible disease is the existence of a human disease factory. Without social conditions that allow the evolution of virulent, transmissible disease, deadly outbreaks are unlikely to emerge.
Deadliness itself isn’t that uncommon: SARS, or severe acute respiratory syndrome, which terrorised China in 2002 and 2003, killed 10 per cent of its victims; Ebola kills 60-90 per cent; untreated rabies kills close to 100 per cent, as does untreated pneumonic plague, caused by Yersinia pestis, the bacterial agent of the Black Death, the worst pandemic in human history. But to be both deadly and efficiently transmissible requires exacting circumstances. Even the Black Death – thought to come originally from Central Asian marmots – must have evolved in a chain of human-to-human transmission to become as lethally and effective as it was.
Fighting existing pathogens is more urgent than hunting for possible new ones – less exciting, but more likely to ease real suffering in the world
So what is wrong with listening to the drumbeat, to the endless calls to protect ourselves against the coming plague – against Ebola from Africa and bird flu from Asia? Is it possible that a huge pandemic could erupt from some as-yet unknown pathogen? Is apocalypse lurking out there, among rats or monkeys, or bats or flying squirrels or birds? The Black Death shows that you can never say never: there might be an animal pathogen out there that, under the right circumstances, can evolve and maintain both virulence and transmissibility among humans as well as animals.
The Central African monkeypox virus (so called because it was first identified in macaques in 1958) has dangerous attributes: like the smallpox virus, it is often deadly, and it’s also a ‘sit-and-wait pathogen’, in Ewald’s terms – highly durable in the outside environment. Yet the evolution of monkeypox into a human disease such as smallpox seems, at this point, unlikely: some strains of monkeypox have transmitted from person to person for several iterations, but the chains of transmission have easily been broken, and the evolutionary process stopped in its tracks.
Instead, people continue to die of human-adapted disease. Malaria kills more than 1 million children annually. Tuberculosis, in its ugliest, drug-resistant forms, is well-entrenched worldwide. Polio, despite our noblest efforts, continues to cripple and kill children. Fighting existing pathogens seems more urgent than hunting for possible new ones – less exciting, but more likely to ease real suffering in the world.
If the Great Plague of Athens tells us anything, it is to avoid social conditions that allow pathogens to evolve great virulence and transmissibility. Preventing disease factories – trench-like warfare conditions, crowded hospitals, enormous refugee camps – is our best protection. While alarmists among us wait for the plague to pounce out of the jungle, it is far more likely to come from inside us, our disease factories and our social world.