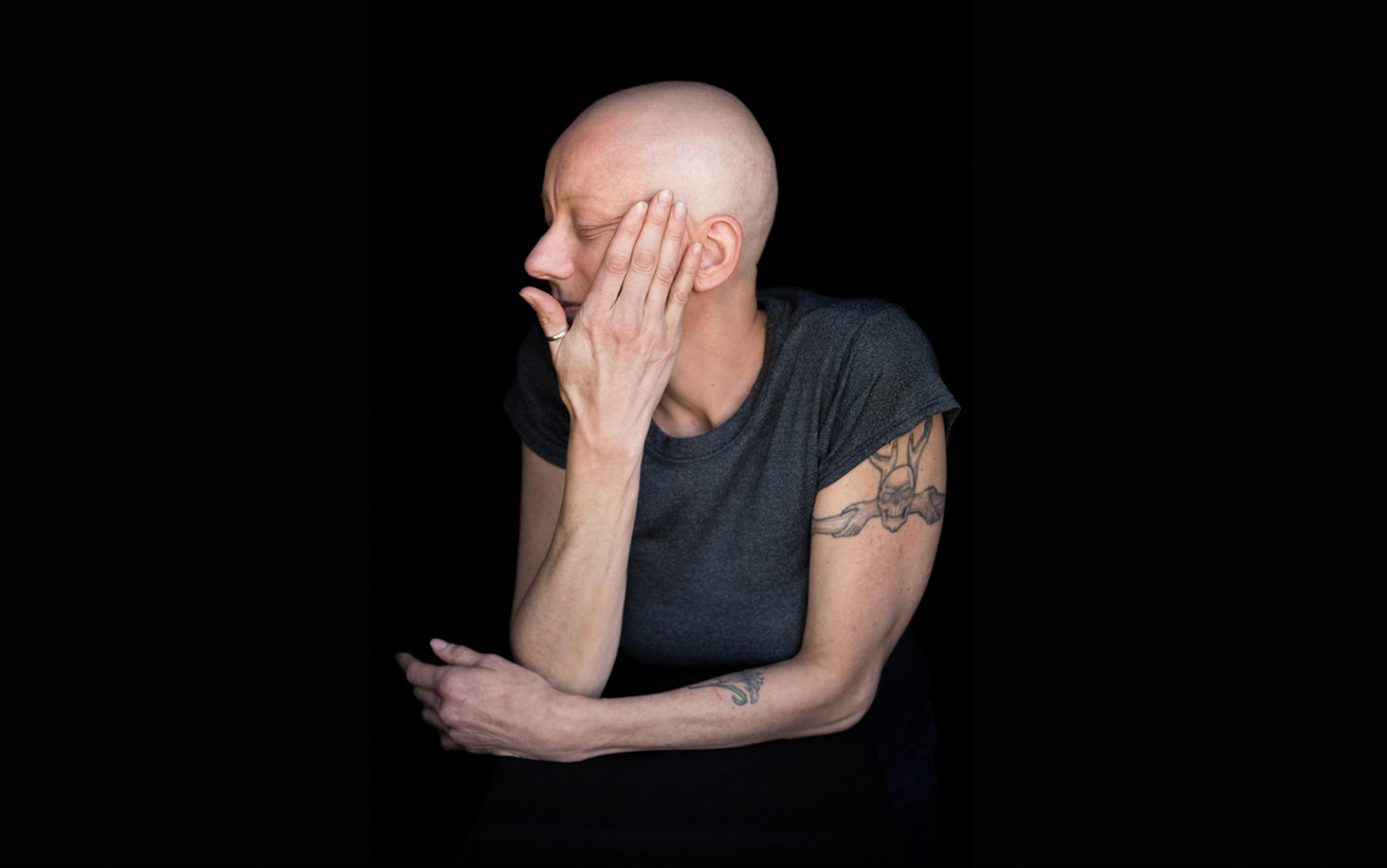
One of us – Joanne Hunt (Jo) – has been largely confined to the house for more than a decade, sometimes bedbound for weeks or months at a time. Jo’s primary diagnoses, hypermobile Ehlers-Danlos syndrome (hEDS) and myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), mean that her daily activities are severely restricted.
Jo had to wait more than 30 years for a diagnosis of hEDS, characterised by joint instability, hypermobility and chronic pain. Most clinicians still struggle to know how to treat it, and the burden has been on Jo to learn about, and figure out, how to manage that condition, which is considered the most commonly occurring variant of EDS, a group of rare inherited conditions.
One of the roadblocks to Jo’s treatment was lack of knowledge among clinicians, creating a devastating obstruction to care – often a problem for patients with rare conditions like EDS. When providers and researchers are able-bodied while patients are disabled, the chasm in lived experience, motivation and immersion in every last nuance of a condition can often be vast. In medicine, the traditional model for researching disabilities repeats itself again and again: nondisabled researchers conduct their studies ‘on’ disabled people as their subjects. While there may be nothing inherently wrong with this mode of scholarship, it carries limitations that should be acknowledged. The fact is: patients can have different priorities from clinicians. They can see things that clinicians may not recognise because they accrue vital first-person knowledge that comes from living with disability or illness. And they are most certainly stakeholders in the research outcome of their own disease.
Given all this, it makes sense to encourage more active patient voices in clinical research. As co-investigators, patients could offer unique insights into their health conditions and ask penetrating questions about treatments and policies. They could help focus practical attention on the development of more inclusive and effective health and social interventions.
While this all sounds great in theory, is there any evidence that healthcare could do a better job if it harnessed the insights and expertise of patients? Patient-researchers are still a novel idea in academia, but emerging evidence shows they offer insights that enhance clinical knowledge. One study in oncology found that investing in patient co-investigators in the design and conduct of clinical trials yielded a 500-fold return. This was because patients offered recommendations that improved enrolment, adherence and retention of participants.
One of the first people to pioneer patient-research was Rosamund Snow, who died in 2017, aged 46. In 2013, she became the first person to obtain a PhD in researching their own condition: in Snow’s case, type 1 diabetes. Her pathway into research began when a consultant at her diabetes outpatient clinic in Oxford asked for help to investigate the clinic’s considerable ‘DNA’ (did not attend) rate, resulting in some widely held clinical assumptions being overturned. For example, pre-existing research on DNA rates across diabetes clinics assumed that nonattendance caused higher levels of HbA1c (glycosylated haemoglobin, a marker of blood glucose control) as typically found among nonattenders. However, Snow’s research suggested that the inverse might be true: some patients with high HbA1c levels did not attend clinic because they feared clinicians judging their ability to self-manage.
‘We think to look in new places, and we spot discrepancies that doctors take for granted’
Snow also investigated how empowerment impacted a patient’s relationship with clinicians. ‘What happens when patients know more than their doctors?’ asked her article, published in the British Medical Journal more than a decade ago. She found that the ‘partial role-reversal of expertise’ created tensions: clinicians who knew less than patients conducting deep research of their own often felt the patients’ knowledge was inappropriate. Without understanding the regimens the patients had learned to make their lives better, the clinicians might end up blocking ‘access to medication and supplies needed to manage chronic diseases successfully’, damaging the patient’s quality of life. Snow emphasised that clinicians had to develop strategies to respect patient expertise so as not to risk harming them.
Later, as an academic at the University of Oxford’s Nuffield Department of Primary Care Health Sciences, Snow taught communication skills and the importance of the patient perspective to student doctors, and worked to embed patient involvement into curriculum design. Among her achievements was a post as patient editor at the British Medical Journal, where she contributed to a radical overhaul of existing protocols and processes for patient-clinician partnerships.
Snow made a lasting impact in the field of type 1 diabetes, in the process changing attitudes toward patient-researchers. The University of Oxford now offers a Rosamund Snow Scholarship for Patient-Led Research. In 2016, encapsulating the value of patient-researchers, Snow wrote: ‘I realised that patients can see things in research that clinicians can’t because we think to look in new places, and we spot discrepancies that doctors take for granted.’
Snow isn’t alone. Liz Salmi – a patient from Sacramento, California who calls herself a ‘citizen informaticist’ – has had tsunami-like ripple effects on patient rights. Diagnosed with a malignant brain tumour 16 years ago, at age 29, Salmi has devoted her energies to promoting understanding about patient access to their online clinical records. A former colleague of one of us (Charlotte Blease), she works with a research unit devoted to understanding what happens when patients read their records: today, she is a crucial member of the OpenNotes team at Beth Israel Deaconess Medical Center, a teaching hospital at Harvard Medical School in Boston.
While many clinicians were sceptical about granting access to online records, in 2021, under new rules enacted under the 21st Century Cures Act in the US, patient access to online records became mandatory. With only a few exceptions, clinicians were now obligated by law to open the records to the prying eyes of patients. Many clinicians resented this development and were fearful that patients would be unable to understand or would become anxious about what they read. They were particularly concerned that sharing records or test results with patients in oncology would pose special challenges.
Salmi seeks to empower both patients and clinicians
However, Salmi used her knowledge as both a cancer patient and a researcher to challenge these assumptions and to reassure providers. For example, she analysed the results of a large-scale survey of US oncology clinicians and patients with access to their records and found that, while 98 per cent of patients thought reading their own records was a good idea, only 70 per cent of oncology clinicians agreed. More starkly, only 4 per cent of oncology patients reported finding their notes confusing, compared with 44 per cent of oncology clinicians who believed their patients would find the notes ‘more confusing than helpful’. In another survey, in which Salmi served as a co-investigator, 96 per cent of patients reported wanting immediate access to their test results, even if they had not discussed them with their provider first.
In her work, Salmi seeks to empower both patients and clinicians. In the years leading up to the new rules, she delivered more than 70 talks. She has published 50 academic papers in top medical journals, and served as a patient-researcher on multiple grants. It required a patient stakeholder, not a researcher without the lived experience of a patient, to shepherd the new policy, though.
Nearly 40 years ago, at age 13, Sara Riggare of Stockholm ‘noticed that my body did not always respond to the signals from my brain or move in the way I wanted it to.’ Because of her early onset symptoms, it would take another two decades for medical professionals to diagnose her with Parkinson’s disease.
An engineer by training, in 2010 Riggare decided to combine her technical expertise with her patient experiences to find superior ways to track her symptoms and find out what strategies worked best for her.
Today, she is a patient-researcher at the Department of Women’s and Children’s Health in Uppsala University, Sweden. She argues that patients acting as self-researchers is a no-brainer: ‘I see my neurologist twice a year, about half an hour every time. That’s one hour per year in healthcare for my Parkinson’s disease. During the same year I spend 8,765 hours in selfcare, applying my knowledge and experience together with what I get from my neurologist to manage a difficult condition as best I can.’
In 2022, Riggare became the first person to gain a doctorate in ‘personal science’ – the revolutionary field in which patients can, and do, conduct research on themselves. At her PhD defence, a member of the opposition committee was a person with Parkinson’s disease – the first time ever this had happened in a doctoral examination. Riggare believed it important that she was grilled for her research by someone with lived experience of the condition.
Her current passion within this area is the field of the ‘quantified self’, which focuses on patients empowering themselves via continuous technological monitoring of their symptoms to better understand and take control of their health. Riggare considers this a better way to manage her own disability. She also believes there is enormous potential for patient-researchers to offer cutting-edge insight into Parkinson’s and other diseases.
She was told: ‘But Sara, wouldn’t it be better if you all just give your data to a proper researcher?’
On the face of it, this elite bunch appears well embedded within health research and academic institutions. They conduct top-tier research, collaborate with academics, and speak to clinicians about improving how care might be delivered. Each one has been published in top medical journals. During her lifetime, Snow published several articles in the British Medical Journal. Salmi has published in The New England Journal of Medicine. Riggare has written for Nature. Collectively, they have received numerous accolades and awards for their work and have collaborated on well-endowed research grants.
However, these accomplishments are largely despite, not because of, their patient status. In her doctoral thesis, Riggare noted:
I started my PhD at Karolinska Institutet [in Stockholm] in March of 2012 and it’s been all but straight-forward. To be honest, if I had known then what I know now about all the issues I would encounter, I’m not sure I would have gone through with it. Of course, the issues that most PhD students inevitably face were not surprising, like having your submitted manuscript – after all the hard work of writing up your study findings – receive a ‘desk reject’ from a journal editor, or the complex process of struggling with wrapping your head around the complicated rules for required academic credits.
What was more unexpected was the resistance from the academic system itself. For instance, when discussing her research with a senior academic researcher, she was told: ‘But Sara, why would patients want to do research on themselves anyway? Wouldn’t it be better if you all just give your data to a proper researcher?’
Riggare didn’t know how to respond:
What did he mean by ‘proper researcher’? It was 2018 and I was hoping to be able to defend my PhD thesis soon. His comment shook me.
Ever measured in her thoughts, Riggare fully acknowledges that there may be times when patients could be biased or mistaken in their thinking about their illness. But, she argues, there is also rigidity in the biomedical ecosystem that needs to be called out, too.
Riggare adds that the motivations for pursuing research can be strikingly divergent:
I have many times been surprised at just how fundamentally different the driving forces can be between ‘regular researchers’ and patient-researchers and not in the way most probably imagine. Many patient-researchers are actually less prone to favouring their own individual agendas than ‘regular researchers’ are, maybe because we know that it really is true that ‘if you want to go fast, go alone, but if you want to go far, go together.’
Describing the challenges for patient-researchers in Nature in 2020, Riggare sums it up: ‘Our contributions are questioned as being unrepresentative, invalid and unobjective.’
Meanwhile, in the US, Salmi’s colleagues at OpenNotes strove to secure for her a faculty appointment at Harvard. Salmi recounts:
Things were looking favourable. Anticipation mounted. The academic rank of ‘associate’ was proposed … It felt like a patient perspective at Harvard Medical School just might become a reality!
‘Except,’ she says, ‘it didn’t.’
Despite her stellar record of publications, Harvard’s offer was conditional on Salmi relocating from California. She declined, so now her researcher role falls under ‘other duties assigned’.
During her lifetime, Snow also wrote about the tensions of navigating a dual identity as a patient and a researcher – and about the myriad ways that medicine unwittingly downgrades the credibility of patients. Having participated in countless ‘public and patient involvement’ (PPI) initiatives, Snow observed that clinicians and researchers frequently framed patients’ inputs as lacking insight. Echoing Riggare’s reference to a ‘proper researcher’, she noted a knowledge hierarchy that persistently placed patient-researchers below what she termed ‘healthy researchers’.
These case studies of patient-researchers operating at the fringes of academia are indicative of ‘epistemic injustice’ in academic health research. The British scholar Miranda Fricker coined the phrase back in 2007 to refer to the varieties of unfairness that arise in relation to knowledge and understanding. She identified two main kinds of injustice. First is discrimination that arises when the words spoken by individuals or groups of individuals are not taken seriously. Even when patient-researchers demonstrate that they bring a novel and original perspective, they risk being discredited.
For example, Riggare’s research agenda was considered not quite worthy, and she was advised to leave the scholarship to ‘proper researchers’. It is worth adding that many scholars working in medical schools have no formal research training either.
Snow recounted hierarchical divisions between patient-researchers and ‘healthy researchers’ that were so entrenched as to exclude patients with PhDs from PPI reference groups. In each case, patient-researchers found themselves demoted as ‘lesser’ and omitted from, as Fricker describes it, ‘trustful conversation’.
Riggare sums it up like this:
One thing about being a patient-researcher in academia is you constantly have to watch your back. And I mean constantly. It takes so little for anyone to question your existence/ability/research/scientific credibility at any time. It’s exhausting.
Fricker identifies a second kind of discrimination arising when there is a collective gap in understanding that makes it hard for individuals or groups of people to communicate their experiences, or to make better sense of them. Imagine trying to tell a story about some fundamental aspect of your life but you and the listener both lack the words to tell the story effectively. This encapsulates a form of discrimination that Fricker calls ‘hermeneutical injustice’, referring to the exclusionary ways in which institutions operate, shutting out some groups or individuals from access to expertise or knowledge-formation activities.
Disability disparities ripple through the education system, right up to the top
As Riggare notes, academia is a tough environment for everyone, but even more challenging when you must manage chronic illness. Salmi was a member of the American Medical Informatics Association but, as she emphasises on her website, she ‘refuses to renew her membership until the organisation creates a discounted membership category for patient informaticians.’
Despite more focus on diversity, equality and inclusion (DEI) in academia, it remains an unwelcoming place for people with disabilities. Disability disparities ripple through the education system, right up to the top. A particularly depressing statistic is the stark educational attainment gap among people with disabilities compared with nondisabled people, with notable disparities occurring at degree level and therefore affecting the pursuit of postgraduate research.
Moreover, as Jo knows only too well, whereas a ‘leaky pipeline’ exists for many historically marginalised groups who are lost from different academic disciplines, there is no pipeline whatsoever for people who cannot leave their homes due to disability or ill health. With three first-class degrees and more than a dozen published papers, Jo has struggled for more than three years to find an accessible PhD programme as a person largely confined to the home.
Regrettably, many disabled individuals who want to pursue research know all too well that the idea of an inclusive academy is a fiction. Yet epistemic injustice is so entrenched that the academy, administrators and even scholars may not notice it.
Remote working policy is just one example of this. As COVID-19 demonstrated, and as the volume of talks clocked up by Salmi illustrated, many researchers can and do work remotely, virtually and with flexibility from home. One recent analysis of 110 studies of more than 45,000 people found more benefits than downsides to remote working – the practice predicted higher worker satisfaction and performance ratings without costs to relationships.
Yet research also demonstrates that doctoral students and academic staff with disabilities were denied similar opportunities for remote working both before and after the pandemic, despite these provisions constituting reasonable adjustments or accommodations under disability equality legislation, such as the UK Equality Act 2010, the US Americans with Disabilities Act 1990 and the US Rehabilitation Act 1973.
Traditional academic healthcare research seems locked in a state of stagnation with respect to understanding the plight of disabled people. This leads to another vicious cycle by preventing deeper, more nuanced research into disability-related themes. Would-be patient-researchers are stifled because they are prevented from fully partaking in research that could advance our collective understanding with potentially positive benefits for disabled people.
How can things change? Flexible, adaptable online access to academia could help. For example, a study of online learning at the University of Derby in the UK, a leading British online education provider, reported three times as many disabled students compared with the British national average.
However, online strategies are not a magic bullet. Technology, including access to digital devices, home broadband and application design, is often out of reach for disabled people. Nor should focus on online strategies be an excuse for ignoring how physical spaces could be transformed to make them more welcoming for people with disabilities.
Mindsets need to change, too. In academia, governing boards, faculty and administrators should become more aware of the needs of disabled students and researchers. Efforts to accommodate and include disabled people, even in what might be perceived as the smallest of ways, could go towards encouraging and sustaining students and scholarship. We also need more cooperation between universities, governments, disability organisations and funders. Many international DEI charters in higher education and research focus on gender and race, but people with disabilities are too often the forgotten, marginalised group treated as irrelevant or unworthy of attention.
Lacking patient insights, the greatest damage is to our collective wisdom
People contend that patient-partnership initiatives are tokenistic, and this may be true. To truly change culture, ‘patient-led’ models have been proposed, where patients lead or co-lead on research from the very outset of investigations, determining what questions are asked and how they are addressed. There are glimmers of hope that patients’ contributions are increasingly being taken seriously.
Rosamund Snow, Liz Salmi and Sara Riggare are hardly the only patients who have contributed to health research. There are many others who have pushed the boundaries of academia, catalysing deeper understanding about disabilities and chronic illnesses. They include Tom Kindlon, Keith Geraghty, Mark Vink, Frank Twisk, Alem Matthees and the late Robert Courtney; they set about investigating the quality of the evidence for four treatments, including cognitive behavioural therapy and graded exercise therapy, for people – like Jo – who live with ME/CFS. These patient-researchers from outside and within the academy challenged fundamental weaknesses in the methodology behind the highly cited and influential ‘PACE trial’ published in 2011 in the UK. Identifying key errors in analysis of the data, they found that established researchers had overestimated the potential benefits of these treatments and had dramatically masked harm. As a result, in 2021, graded exercise therapy was removed from recommendations set by the National Institute for Health and Care Excellence – the UK’s organisation for setting national guidance on health and social care.
Finally, we must honestly acknowledge that this pursuit is both a personal and an intellectual ambition for us. For one of us (Jo), life-long experience of how illness can be compounded by disability denial and discrimination has convinced her of the need for a radical paradigm shift in (bio)medical care and psychotherapies, where disability is understood as extending far beyond the individual and into society. It is personal to Charlotte, too. She has two siblings who live with the rare congenital disease myotonic muscular dystrophy, one of whom waited decades to be diagnosed. Perhaps it comes as no surprise that we both believe that finding new ways to listen to patients’ voices is crucial if healthcare and medical research is to serve its function effectively.
The academy can and should do more to promote diversity and inclusion among disabled researchers. Lacking patient insights, the greatest damage is to our collective wisdom. If we truly prize viewpoint diversity, then we must embrace the voices and insights of under-represented disabled people who could add significant value to academic and public life – including a deeper understanding about the very place where they should feel welcome: healthcare.
If the academy were truly open to patients as co-investigators, professors and researcher leaders, healthcare could solve problems it never knew it had. It could also orient itself to redefine care in ways that health systems and societies have not yet imagined. We believe that such a future would not only be fairer and more enlightening but also a more fascinating and hopeful place to live.