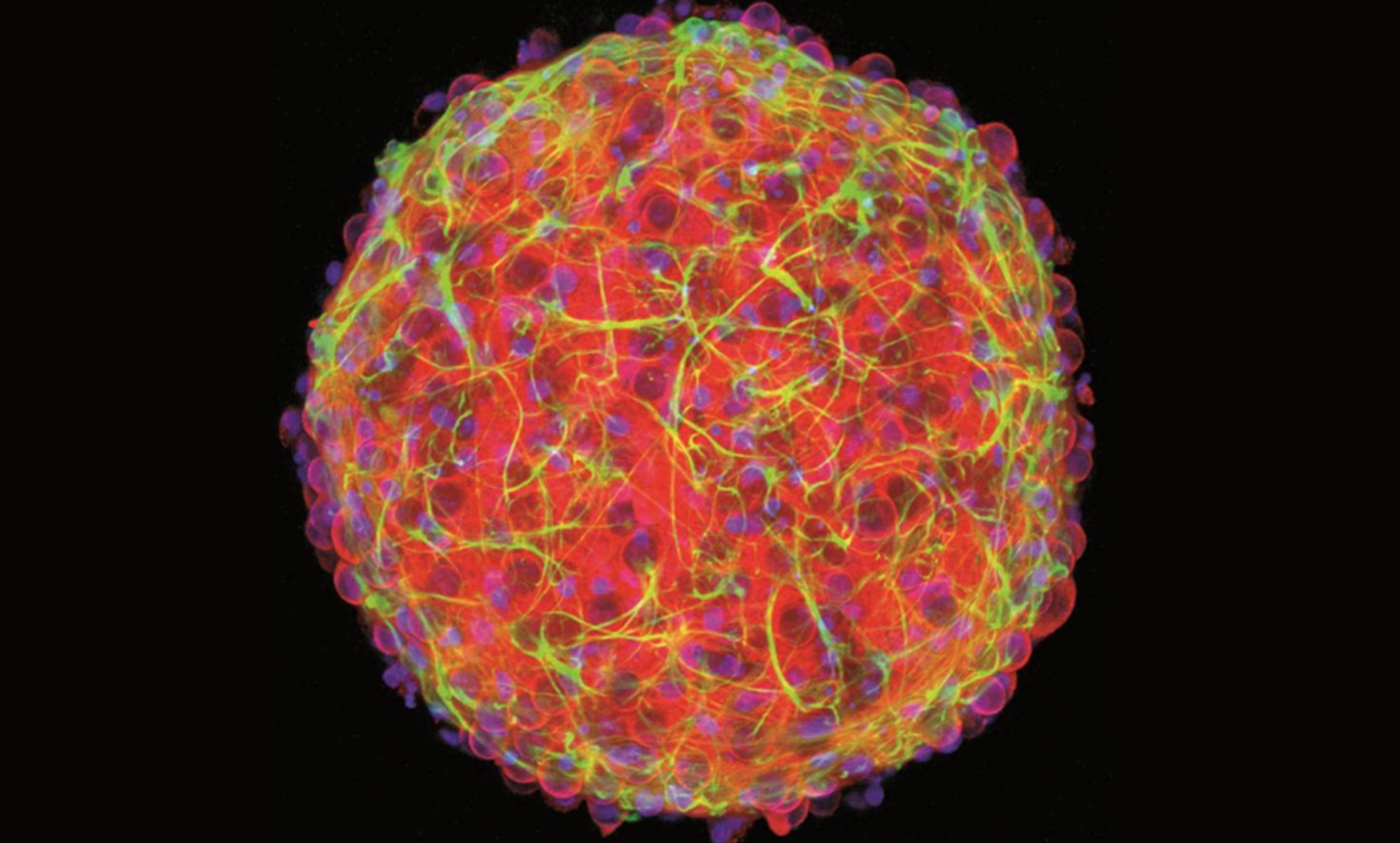
Courtesy Hoffman-Kim Lab/Brown University
Last year, Diane Hoffman-Kim and several researchers at Brown University in Rhode Island created a tray of mini-brains in the lab. While the new brains lacked the complex architecture to be fully functional thinking brains, they were nevertheless small bundles of nerve cells about 200 micrometres in diameter that emitted electrical impulses, much like our own brains.
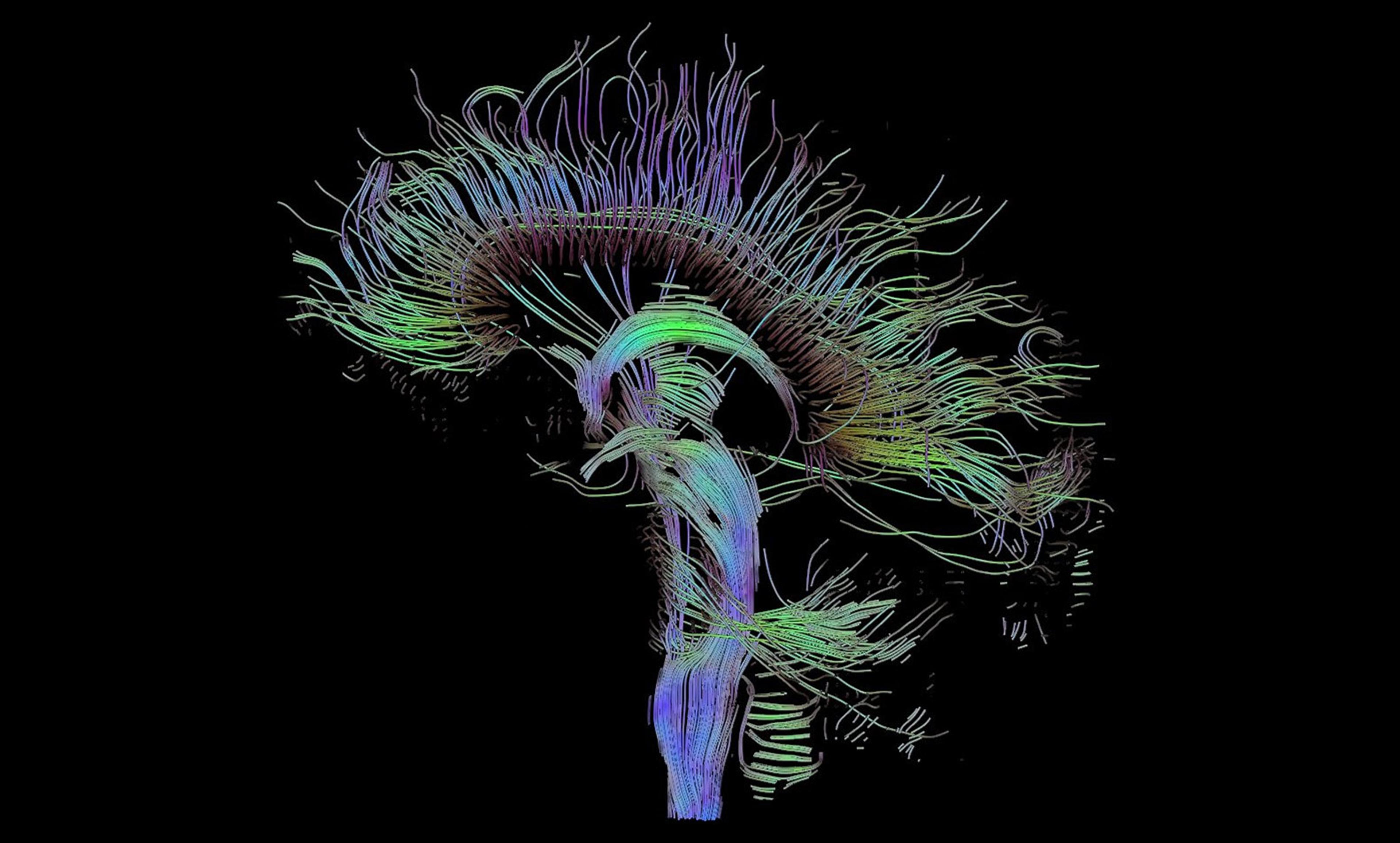
Hoffman-Kim and her colleagues were not the first to create brain-like structures in the lab, but their model, among the most sophisticated such structures ever developed, has already been used to simulate traumatic brain injury and Alzheimer’s disease, along with testing the impact of various drugs. The approach used by the Brown University researchers offers a model that simplifies the brain to its most critical components, including neurons, neural stem cells, astrocytes (which provide nutrients to nervous tissue and help repair the brain after a traumatic injury), oligodendrocytes (which protect nerve cells), microglia (which help direct the immune system in the central nervous system), and other molecules that help make up the structure of our brain (such as proteins).
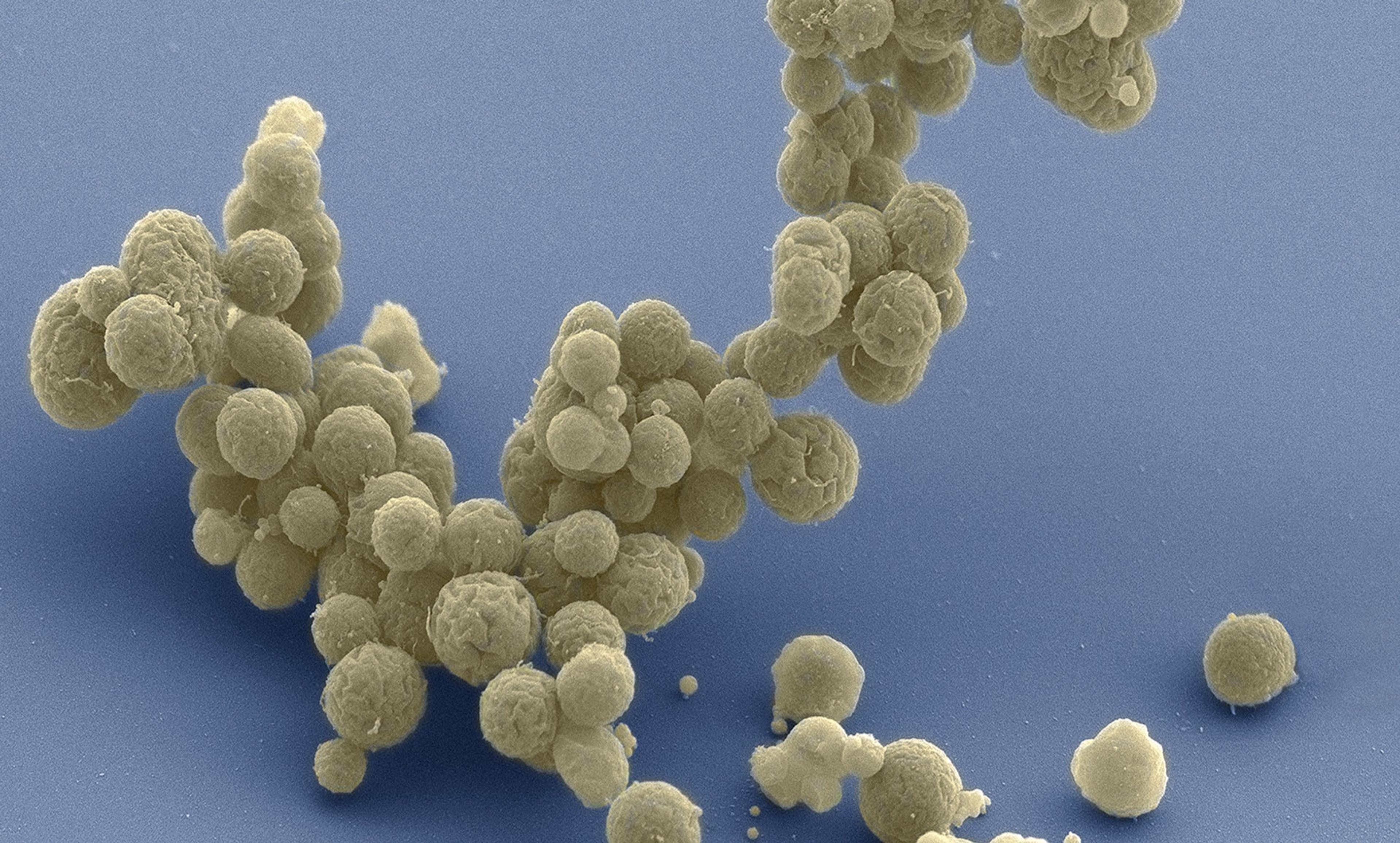
These simplified brains are so affordable to create that Hoffman-Kim estimates each brain costs about 25 cents. These inexpensive mini-brains are part of a growing movement called ‘organs on a chip’, where scientists create mini-organs (hearts, kidneys, brains) from human-derived stem cells. The organs are generally created from induced pluripotent stem cells, created through a process that tricks regular human cells (obtained from a simple cheek swab or blood sample) into behaving like embryonic stem cells. This neatly sidesteps the ethical issues of taking stem cells directly from human embryos, but makes it possible for researchers to create mini-organs from the unique cells of individual human beings.
‘The idea is if we can get a skin sample or a blood sample, we could basically make a dish of about a hundred brains,’ Hoffman-Kim said. Scientists could then test these brains to analyse the effects of certain drugs for each specific patient and track developments of brain-related disorders.
Moving towards a workable model for our brain is the next frontier for personalised medicine. Our brains are crucial to our health: they control everything from memory and emotion to immune responses. Yet, encased in the protective fortress of our skulls, our brains are also one of the least understood organs in our body. As mini-brains become easier to create, doctors could use these models to better understand how each patient would react to a drug, or how their conditions could progress without ever having to access the patient’s actual brain. Doctors could take samples of a patient’s cells, use them to culture several mini-brains, and test the effects of different drugs on those brains to see how the patient would react to the drugs.
In addition, these brain models help to address the limitations that personalised medicine currently faces. Much of today’s personalised medicine research focuses on genetic information. Yet scientists know very little about the relationship between gene markers and disease, or reaction to drugs. Most of the information we have comes from studies that measure the correlation between certain gene markers and certain conditions rather than causation. On the other hand, replicating a patient’s organ in the lab environment gives scientists an opportunity to see exactly how it would react in current situations.
Of course, scientists still have to answer a lot of questions before individual lab-grown mini-brains become a reality. One of the major questions is understanding which of the brain’s complex components is necessary to sufficiently mimic the human brain and which ones we could do without. How much of the brain’s complex architecture do we need to mimic the effects of Valium, for example? How much of the glial cells, the non-neuronal cells that provide protection for neurons, do we need to recreate Alzheimer’s? ‘It all boils down to figuring out which models to use,’ said Hoffman-Kim.
But her work shows that we’re close. Her team is already able to mimic the effects of stroke with their 25-cent mini-brains. Pretty soon, they’ll be able to mimic the effects a stroke would have on your brain before you have one yourself. And even more exciting – they’ll be able to test treatments that might work best for you without putting your actual brain at risk.