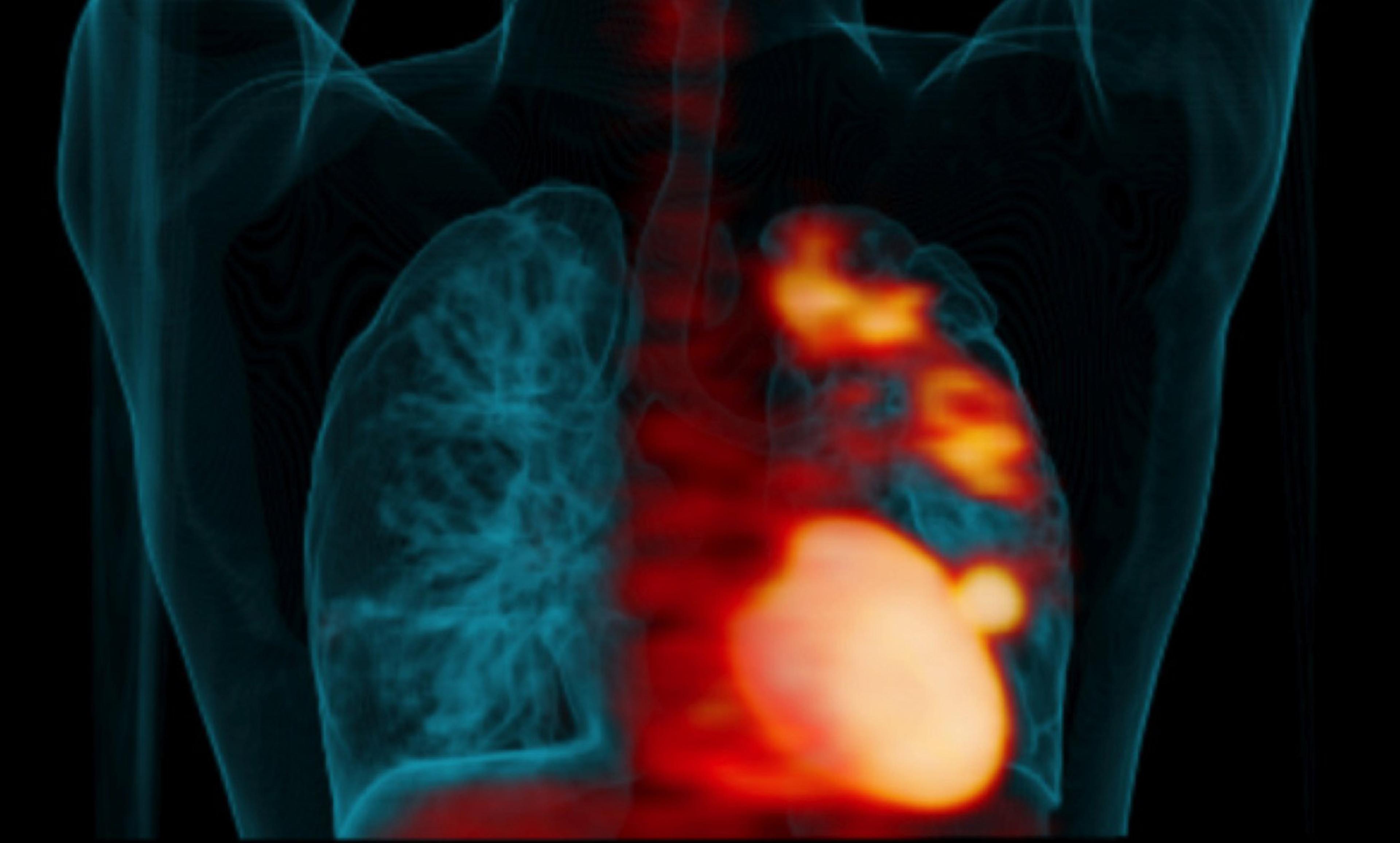
Lung scan showing ‘hot spots’ of TB infection. Photo courtesy UPMC Pittsburgh
We live in a world where continuous innovation is normal and unremarkable. We expect a constant stream of newer and better things to power an ever-rising tide of growth and prosperity. But this was not always the case. From the dawn of history until about 1800, everyone was a subsistence farmer, everyone was poor, and there was precisely zero growth in the income of the average world citizen. The innovation economy is a singularity in the history of humanity. Control of infectious disease is the portal through which we reached the singularity.
Innovation happens when large numbers of people gather in close proximity and expose each other to their ideas and inspirations. Innovation depends on personal contact and social networks. The dependence of innovation on the density of social interactions can be accurately described by simple equations: the same equations that describe the spread of disease epidemics.
We shouldn’t be surprised, then, that the control of infectious disease was essential to developing our world of sustained innovation. Before this control, the necessary concentration of minds also resulted in the spread of diseases that crippled innovation. The largest cities of the Enlightenment world in 1800 had populations of only a few hundred thousand. Their inhabitants died faster than new citizens were born, and they sustained their modest sizes only by continual migration from the countryside.
Of all the diseases that decimated emerging cities, tuberculosis (TB) was the worst. ‘Decimation’ – the taking of one in 10 – is an understatement. TB accounted for a quarter of all deaths in European and North American cities in the early 19th century, killing 80 per cent of those it infected. Like AIDS today, TB was so destructive because its usual victims were young adults, the most dynamic, productive and innovative members of society. TB is the reason why so many Georgian and Victorian novels feature orphans and orphanages.
The Golden Age of Public Health – roughly from 1860 to 1960 – very much overlapped with the Golden Age of Innovation, and this is no coincidence. Clean water and food, along with vaccines, made large dense cities habitable, and enabled unprecedented levels of innovation and creativity. The rapid drop in childhood deaths freed women from the necessity of bearing many children and nursing them through repeated medical crises, and women responded by demanding education and a role in public life. All of this was new in human history.
TB deaths fell dramatically during this time, as did all other infectious diseases. From 1860 to 1950, deaths from infectious diseases fell by nearly 90 per cent in England and Wales, and by similar amounts in other industrialised countries. This decline occurred prior to the general availability of antibiotics. It can confidently be attributed to the implementation of public-health measures, principally the provision of clean water and food, and the development of vaccines. We know how to prevent the spread of infectious disease, a comforting thought in a world in which antibiotics are beginning to lose their invincibility.
There is one exception to this tidy story: we don’t really know why TB declined. Some of the decline can be attributed to the pasteurisation of milk, through which the bovine form of TB spread. TB is not otherwise spread through food, and so cleaning up slaughterhouses and developing refrigeration had no impact. TB, unlike yellow fever or malaria, is not transmitted by insects, and so draining swamps did not impede it. Clean water prevents the diarrhoeal diseases that carried away so many children, but does not prevent TB, which is spread from person to person. Vaccines halted killers such as diphtheria and smallpox, but the TB vaccine is not very effective.
Historians of medicine have proposed other causes. Once the contagious nature of TB was established by the German physician Robert Koch in 1882, quarantines and sanatoria were established to break the train of transmission. But these efforts were inconsistent and sporadic, and many scholars doubt whether they played more than a minor role in TB control. Because the TB death rate was so high for so long, natural selection for innate immunity has also been proposed to account for its decline, and there is some evidence supporting this view.
Thomas McKeown, a British physician and medical historian, was skeptical of all these explanations. In the 1960s and ’70s, he published a series of works arguing that TB was principally – perhaps purely – a social disease, one that responded not to medical or public health interventions, but to the improved living conditions of the population. McKeown’s argument was that TB deaths began a steady decrease well before that of other transmissible diseases, and that the rate of decrease correlated closely with measures of social wellbeing and not at all with the introduction of various public health and medical interventions. He became, despite his medical training, something of a medical nihilist, arguing that all medical interventions are worthless, and that the funds dedicated to R&D and the development of Britain’s National Health Service would be better spent on feeding and housing the poor.
McKeown’s thesis has an intuitive appeal. TB largely disappeared from prosperous countries and is now considered a ‘disease of poverty’. But subsequent scholarship, resting on more sophisticated analyses of demographic and economic data, do not support McKeown’s claims, and his thesis is now considered largely refuted. However, no other explanation has gained widespread acceptance in its stead.
The arrival of anti-TB antibiotics in the late 1940s seemed to render these arguments irrelevant, of no interest to anyone save medical historians. With the advent of streptomycin, then isoniazid, then rifampin, TB – for the first time ever – could actually be cured. Its chain of transmission could be broken without resort to quarantine. Nor was there a need to engage in the daunting task of providing adequate food and decent housing to the world’s poor. Antibiotics were effective and cheap. If they could be given to every patient, then the threat of TB to human health and civilisation could be ended, perhaps forever.
The emergence of antibiotic resistance in TB thus constitutes a singular threat, different and much greater than the threat posed by the so-called ‘superbugs’. Most multiply-resistant bacteria display reduced virulence – defined as the ability to infect and sicken a host – and rarely infect otherwise healthy people. For most of these pathogens – MRSAs, CREs, VREs, ESBLs – the principal risk factors for serious infections and death are old age, hospitalisation, immunosuppression, and recent antibiotic use. They attack the old and sick, not the young and healthy.
Multiple drug-resistant (MDR) TB is different; its acquisition does not make TB less virulent. Most victims are between 25 and 45 years old, in what should be the prime of life. The main risk factors for infection with MDR-TB are previous TB treatment and refugee status. MDR-TB is treatable, but treatment is arduous and expensive, and often not effective. Half a million people fell ill with MDR-TB in 2015, and only a quarter of these received adequate treatment, getting well.
Most organisms become less virulent as they spread, but it is plausible that MDR-TB will become more virulent in high-density settings. If this occurs, we are in deep trouble. We have no credible Plan B for containing an outbreak of TB strains that are both drug-resistant and more virulent. We cannot quarantine millions of people. Better public sanitation will do no good because the disease is spread person-to-person by coughing, sneezing or even speaking. Perhaps natural selection has made us less susceptible to infection than our ancestors, but this is a hope, not a plan.
At a certain tipping point, TB could make our progressive, innovation-driven society unsustainable. The same interactions between ‘makers’, who we rely on to drive our economy, will also spread a deadly, difficult-to-treat disease. The hardest-hit among us will be young adults whose lives and careers are cut short, causing immense strains to our social fabric. Our highly interconnected economic system that has reduced poverty to the lowest levels in history will begin to collapse, creating a positive feedback cycle of more disease and disruption.
None of this might happen of course. But consider a worst-case scenario: the new strains of TB combined with climate-driven crop failures, resulting in mass migrations. The result could spawn an essentially unstoppable epidemic that would put an end to the modern economy. We are more vulnerable than we realise; the White Death might walk among us once again.