Noah Wolfson was just 12 when he learned he had cancer. What made his case unusual was his father’s response. Phil Wolfson, a psychiatrist in Marin County, California and veteran 1960s activist, mined not just his training as a physician but also his connections to countercultural healers and psychedelic medicine pioneers to help his son.
Even with these transformative tools at Wolfson’s disposal, the diagnosis and its aftermath shattered this family. There was nothing normal about navigating the menu of often excruciating treatments meant to save Noah’s life under an ever-present cloud of doom. The family struggled with a paradox of modern medicine that affects an ever-growing number of people: therapeutic advances designed to cure life-threatening illnesses can leave survivors traumatised by their medical journey.
A diagnosis of cancer or other potentially fatal illness can trigger intense anxiety and despair. The initial shock, compounded by the pain and dread of enduring one mutilating procedure after another, can prove overwhelming, both to patients and their loved ones. Add in the fear of recurrence, relapse and death, and reactions can range from transient post-traumatic stress disorder symptoms to full-blown PTSD.
Wolfson’s harrowing experience with his son’s illness gave him a deeply personal view of the psychological scars of life-threatening diseases. ‘I share it often with my patients because I know it,’ he tells me.
In turn, Wolfson’s patients helped him recognise the broader clinical implications of his family’s ordeal. And it was through this recent work, combining MDMA (aka ecstasy) with psychotherapy during a three-year clinical trial, that he documented the devastating psychological impacts that a life-threatening illness can have on patients. ‘I had the view of 18 people who’d been traumatised in various ways,’ he says, ‘how they’ve been hurt and damaged from diagnosis through treatment and recovery.’
The range and severity of traumas that emerged convinced Wolfson of the need to recognise a new diagnosis: PTSD-life-threatening illness (PTSD-LTI).
PTSD is most commonly associated with military combat, sexual assault, accidents, and disasters. Exposure to such traumas triggers a flood of hormones that crank up blood pressure, heart rate and energy levels, which help muster the appropriate reaction to imminent threat. This fight-or-flight response is critical for survival but can turn dysfunctional and lead to PTSD after the threat has passed.
There’s little doubt that being diagnosed with a deadly disease is highly stressful and potentially traumatic. Yet controversy has dogged the PTSD definition and criteria since 1980, when the term was formally introduced as an anxiety disorder in the third edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III), the psychiatrist’s classification handbook. Examples of traumatic stressors, or events, that could cause PTSD included a natural disaster, serious injury from an accident or deliberate act (such as assault or torture), and military combat. Life-threatening illness was added as a traumatic stressor in the revised DSM-IV (1994), and then reclassified in DSM-5 (2013) as a stressor only when it involved a ‘sudden, catastrophic event’ such as waking up during surgery.
MDMA ‘opens the doors of the heart and removes some of the blocks to feeling and suppression’
Core symptoms include intrusive nightmares, flashbacks or other memories of the trauma; conscious avoidance of places, people or situations related to the event; altered mood and cognition such as irritability, an exaggerated sense of guilt or shame, and memory problems; and hyperarousal, or the inability to relax, leading to panic attacks, angry outbursts, and insomnia.
Therapists have long known that MDMA, outlawed in 1985 as having no medical use and a high potential for abuse, melts defences and eases anxieties while boosting mood and trust – key ingredients for successful therapy. The drug works partly by dissipating the crippling fear that prevents people from revisiting a trauma, a necessary step in learning how to live with it. ‘It opens the doors of the heart and removes some of the blocks to feeling and suppression,’ Wolfson says, making it easier to tolerate deeply distressing memories and emotions.
Feeling unburdened, Wolfson’s patients were willing to plumb the depths of their psychic pain in profound ways, looking at how the disease disrupted their lives, self-worth, and personal and professional interactions. Their ability to confront their worst fears helped Wolfson chart a therapeutic path to ease their suffering and anxiety.
A PTSD diagnosis has traditionally hinged on whether specific traumas could produce the disorder, but Wolfson thinks PTSD-LTI merits its own diagnostic category. That would help medical professionals, from doctors to hospitals and insurance agents, recognise that a life-threatening illness can harm the mind as well as the body, and that some patients might need more resources to handle their situation. The biggest beneficiaries, he says, would be those who are ‘living under the Sword of Damocles of relapse and death’.
Wolfson missed the signs of Noah’s cancer at first. Medical training didn’t prepare him to imagine that catastrophic illness could befall his own son. But the time came when he could no longer ignore the unexplained bleeds, headaches and bouts of extreme fatigue. He took Noah to a colleague, who drew a blood sample and called in a paediatric oncologist, who delivered the awful news.
A healthy person should have 150,000 or more platelets, he said. Fewer than 20,000 is life-threatening. Noah had 14,000. The medicines would make him very, very sick, the doctor explained, but they were critical to his survival. ‘Diagnosis, risks, and the road to recovery – in two mind-numbing minutes,’ as Wolfson would later describe the appointment.
Rob Cole had a similarly disorienting experience. He had a thriving practice delivering babies in Walnut Creek, California, when a woman noticed a spot on the top of his head. An oncologist soon confirmed his fear: melanoma, Stage 2. Surgeons removed a wide section of tissue around the lesion along with a ‘sentinel’ lymph node that would reveal if the cancer had spread. The node was negative, and Cole was told he had an 80 per cent chance of survival. After his first operation, he felt like he was floating in space, waiting for someone to call and ask how he was doing. But the call never came. Cole was terrified that the melanoma would return.
And it did, spreading to his neck. Cole endured what’s called a radical neck dissection, which removes several groups of lymph nodes and sections of muscle, jugular vein and the nerve that controls the right arm. Then he started radiation along with a course of interferon to boost his immune system’s response to the cancer. He devoured the scientific literature and realised his chances of survival weren’t great. And without the use of his right arm, he couldn’t deliver babies any more. Word spread that his cancer had returned. ‘I literally had to sell my practice in a week because people were leaving, knowing that I was a dead man walking,’ Cole says.
A year and a half later, his melanoma had progressed, yet he felt oddly relieved: ‘I was so happy when I became a Stage 4 patient because I realised my body was not going to be mutilated any more. I would be getting systemic treatment, and would not have to bear the assault of a scalpel again.’ Then Cole received trailblazing immunotherapy at the National Cancer Institute (NCI). For one treatment, he had to let a tumour grow to the size of a golf ball so clinicians could harvest his immune cells, screen them for anti-tumour activity, propagate those cells in the lab, and infuse them back into his veins. The tumour was disturbing to see and touch, and the thought of cancer infesting his body filled Cole with terror ‘every minute of every day’.
‘As medicine advances, we have more survivors. But those survivors carry trauma to their graves’
Sleep brought relief, but fear would return with the ferocity of a caged lion as soon as he woke up to the tumour on his arm and the reality that he had Stage 4 cancer and just months to live. ‘That is terrifying,’ Cole says. ‘That kind of fear stays with you, even after the tumours have receded.’
Then one day when he was waiting for scan results at the NCI, the doctor shut the door. ‘When the scan results are good, the door stays open,’ he says. The memory of the door closing still brings him to tears. ‘It’s a moment when I was told they had no treatment left for me and I was on my way out.’
Finally, Cole tried another drug, ipilimumab, designed to jumpstart anti-tumour immune responses, and his disease stabilised. ‘That’s been close to eight years ago,’ he says. ‘So I have survived.’ As traumatic as it is to realise that death is in play, Cole says, it can also be very focusing. ‘Many people say that their cancer diagnosis was one of the best things that ever happened to them.’
The struggle to come to grips with a trauma can transform one’s outlook, engendering a new appreciation for life and relationships, and heightened resilience in the face of adversity. Psychologists have been debating the existence and prevalence of ‘post-traumatic growth’ – a modern version of Friedrich Nietzsche’s maxim ‘That which does not kill us makes us stronger’ – since they began studying it formally in the 1990s.
Although a diagnosis can bring benefits, Cole says, ‘you are in a state of anxiety at all times.’ He can’t shake the thought that any aches and pains, normal for his 67 years, might be new signs of his body’s betrayal. Today, he practises palliative care at a hospice. He knows the patients are probably floating in space, too, needing specialised care to manage their distress.
He believes no one should leave an oncologist’s office with a cancer diagnosis without a referral to someone trained to manage the anxiety and trauma that inevitably shadows the course of treatment. But that’s not what happens. ‘As medicine advances, we have more survivors,’ Cole says. ‘That’s a good thing. But those survivors carry trauma to their graves, and we haven’t recognised that it’s a disease process that needs treatment.’
Before PTSD entered the DSM-III (1980) as a single disorder with a constellation of symptoms caused by diverse traumas, researchers had given each traumatic event its own name – post-Vietnam syndrome, concentration-camp syndrome, rape-trauma syndrome, and so on. For a long time, therapists held that people traumatised by different horrific events could respond to the same types of treatments, a combination of talk therapy, prolonged exposure to the trauma to help people tolerate it, and medication.
PTSD is now classified as a ‘trauma and stressor-related disorder’, along with four other conditions, including adjustment disorder, which like PTSD involves a fixation on an event and failure to adapt to it but stems from a major life change, such as divorce or job loss, rather than a life-threatening trauma.
For years, researchers reported that cancer patients had intrusive thoughts and avoided reminders of their disease, two core symptoms of PTSD, says Matthew Cordova, codirector of the Early Intervention Clinic at Palo Alto University and an expert in cancer-related traumatic stress. That’s why experts added life-threatening illness as a precipitating cause of PTSD in DSM-IV. A slew of studies investigating cancer and other medical stressors followed, leading to DSM-V’s assertion that life-threatening illnesses are ‘not necessarily’ a traumatic event. These changes, along with the decision to require ‘sudden, catastrophic events’, Cordova says, were based on studies that used strict diagnostic criteria rather than a patient’s own assessment.
For many, hearing the words ‘You’ve got cancer’ is a sudden, catastrophic event. Yet the catastrophe of cancer is not relegated to an event in the past like a car crash or violent assault might be. Cancer morphs into an ongoing nightmare as chronic as the disease itself, with noxious treatments, uncertain outcomes and routine follow-ups serving as their own traumatic stressors. Patients must endure protracted stress that evolves with the disease, one day dreading what their test results will show, the next wondering what new torture their doctor will recommend, and always fearing, like Cole, that every little twinge signals metastasis.
Estimates of PTSD among cancer survivors vary depending on the method used. In a 2017 Lancet Psychiatry review, Cordova and colleagues found the syndrome in about 6 per cent of patients, using the strictest diagnostic criteria, and about 28 per cent of partners, based on self-reporting (which tends to yield higher results). With nearly 17 million cancer survivors in the US as of January 2019, that means more than a million could have PTSD – and that’s not counting the many millions who’ve survived a stroke, serious burn or other potentially fatal illness.
‘People with trauma feel like the house is on fire … It can be very exhausting’
Still, experts disagree if PTSD is the best label for people’s response to a life-threatening illness. Cordova finds it a useful lens because it helps clinicians support and treat patients by encouraging them to process what they’ve been through and address how it’s changed their outlook, anxiety levels, self-image, view of the future and of the world. ‘Those things are very consistent with how we treat PTSD more generally,’ he says.
‘People with trauma have this super-uncomfortable experience when they are revisiting the trauma,’ says Dianne Shumay, director of psycho-oncology at the Helen Diller Family Comprehensive Cancer Center at the University of California, San Francisco. ‘They get flooded into this experience and it feels like the house is on fire and they have to do something about it right away. It can be very exhausting to react and respond to things on an ongoing basis with that level of physical response.’
Cancer-related PTSD is often missed by medical teams, according to a 2019 paper in the Canadian Oncology Nursing Journal, impairing the quality of life and recovery of patients who avoid check-ups or follow-up scans because they’re too stressful. Because trauma can overstimulate the nervous system’s fight-or-flight response, it primes the body to overreact to stimuli associated with the trauma. A pink ribbon might trigger distressing memories of a fateful mammogram for a breast cancer patient, just as a backfiring car evokes gunfire for a combat veteran.
For all the studies about PTSD related to life-threatening illness that followed its inclusion as a stressor in DSM-IV, research investigating how best to treat it remains sparse. In his Lancet Psychiatry review, Cordova cited a few studies showing that talk therapy reduced breast cancer patients’ intrusive thoughts, but cautioned against using general PTSD treatments for patients with cancer-related PTSD, where trauma is ongoing. ‘For some, it’s less intrusive thoughts about what they experienced and more intrusive thoughts about having to go through it again,’ he says.
PTSD can also lead to ‘excessive rumination’ or indecisiveness in cancer patients who worry about making the wrong medical decision. Encouraging patients to become actively involved in their treatment can help manage these symptoms, and reduce avoidance behaviours that undermine their treatment.
Wolfson found that PTSD takes different forms when someone is struggling with life goals unmet, fear of ‘unbeing’, and denial that their life could be cut short. Here, sufferers could benefit from intensive therapy assisted by MDMA – or ketamine, another drug that opens up clients. Several outcomes measure success, including whether patients recover a sense of vitality, make peace with their limited future, and come to terms with their fear of dying.
While it’s important not to pathologise conditions, Shumay says, a formal diagnosis could make a strong statement to the field that cancers and other life-threatening illnesses can and do cause PTSD. ‘Then it’s more obvious that this is a risk.’
That would give cancer-related PTSD treatment the attention it deserves. The bottom line, Cordova says, is to provide these services, ‘no matter whether we call it PTSD or not.’
Five weeks after Noah was diagnosed with leukaemia, Wolfson wrote in his journal: ‘He is touch sensitive; emotionally sensitive; depressed; weak; unmotivated to fight his illness; motivated to fight with us.’ The pain was infectious, Wolfson noted, passing into Noah’s mother as suicidal despair and leaving his father in a ‘blacker than black hole’.
Noah kept his own journal, parts of which were published in Family Circle magazine in 1989. ‘I can’t deny the fact that this disease is wiping out whole portions of my childhood and replacing it with nightmares, pain, and misery,’ Noah wrote after his first relapse. He found the catheter implanted in his chest particularly upsetting, ‘an inescapable physical feature, which makes me ever aware of my situation. Though it works to save my life, it endeavours to hinder it.’
The chemotherapy didn’t prevent another relapse. Noah opted for a bone marrow transplant, which failed to take. He died in 1988, three months before his 17th birthday.
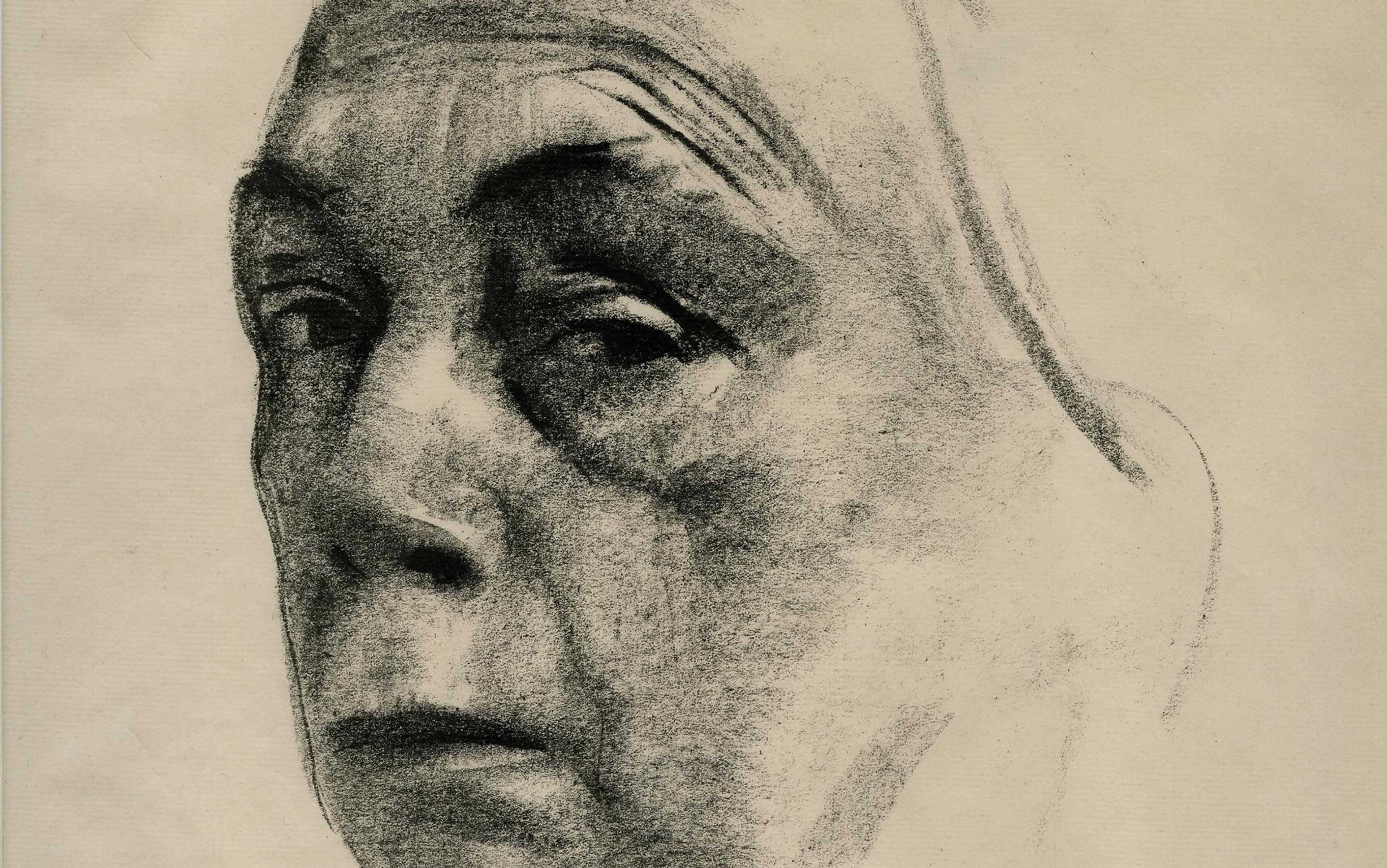
Decades later, once-favourite haunts still evoke catastrophe for his father. Noah’s lip started bleeding uncontrollably on the way to Tahoe, a drive now booby-trapped with memories of fear and foreboding. ‘Many years after these events, I sense each traumatic spot beginning to shimmer in consciousness before its arrival on the road,’ Wolfson wrote in Noe: A Father-Son Song of Love, Life, Illness, and Death (2011), using his son’s nickname.
‘We need a lobby of survivors who say: you got us this far, but didn’t attend to the issues that make life worth living’
‘I’m a PTSD by proxy,’ he told me. ‘It’s a long time, but it’s still there.’ Losing Noah ‘sensitised me in a very unfortunately deep way to loss,’ he says. ‘But that only puts me in a large group of people who’ve had profound losses.’ I’m always feeling people’s losses, their sense of pain and suffering. That’s what my life’s work has been about. How to heal that as much as possible.’
Ketamine and MDMA have been indispensable tools in that work, partly by altering patients’ consciousness to allow for more penetrating explorations of trauma, and partly by transforming the therapist-patient interaction. Psychedelics send patients on a profound, unfamiliar inner journey where long-suppressed thoughts often arise spontaneously. That means therapists must spend hours helping patients process what emerges, and stay with them as the drug wears off. Unlike the ‘50-minute’ hour that dominates commercial psychotherapy, sessions can last up to four hours with ketamine and eight hours with MDMA, Wolfson says. Conventional therapy can produce results too, he adds, ‘but it tends to be more rapid with altered states, and it tends to be deeper.’ People in his MDMA-assisted psychotherapy study described numerous debilitating responses to their illness. Some were common to most PTSD sufferers, including feelings of despair, being hypervigilant, sad, withdrawn and less enthusiastic about normally pleasant pastimes. But many were specific to having a deadly illness, including envy of others’ wellbeing, worries about leaving a mark, nightmares about treatments, and fear of independence loss, relapse and death.
MDMA has proven so effective that the US Food and Drug Administration recently gave it the green light for patients outside of a formal study through a ‘compassionate use’ programme. Yet MDMA’s reputation as an illicit drug means that PTSD sufferers who fail to respond to standard therapies are more likely to find therapists using ketamine instead.
Cole is thinking about bringing ketamine into his hospice practice. In contrast to antidepressants such as Prozac that patients take every day, ketamine provides long-lasting relief after three or four sessions without ‘radically altering their daily neurochemistry’, he says. He’s gone through three sessions of ketamine-assisted psychotherapy himself to manage the lingering effects of his struggle with melanoma. ‘It’s been life-changing.’
Wolfson hopes the new diagnosis will inspire novel therapies with a new cadre of professionals attuned to life-threatening illness. ‘If we’re going to do this,’ says the 1960s warrior, ‘we need a lobby of survivors who say: “Here we are. You got us this far, and a bunch of us are really hurting. You gave us more life, but you didn’t attend to the issues that make life worth living.”’