Auguste Deter died on the 8 April 1906, aged 55, after spending the last years of her life in a psychiatric hospital in Frankfurt, Germany. A photo of her from 1902, after she was institutionalised, shows a woman in a white gown, in a messy bed with her knees drawn up to her chest. She isn’t looking at the camera, and looks lost and bereft. Deter was admitted to hospital because she had a paranoid suspicion that her husband was having an affair, and her memory was starting to decline. During the last years of her life, Alois Alzheimer was her doctor and he took copious notes. After her death, he performed an autopsy on her brain and identified the amyloid plaques and filament tangles that define the disease from which Deter had suffered, and he gave it his name.
The name Alzheimer lives on, and much is known about his life, but Deter has been reduced to her medical notes, written by others, a record of her losing her words, her knowledge of herself and her ability to describe her identity.
More than 100 years later, just like Alzheimer, I collect patient’s stories, examine people and test them, to try to label and categorise. In my role as a doctor, I try to reduce a life lived – symptoms that vary between every person, a cognitive disability that will have a different impact on each individual’s life – to a binary: dementia or not dementia.
How do I compare a retired, 80-year-old male academic with an 80-year-old woman who had only two years of education because she lived through the Greek civil war? How do I compare a woman who does all the shopping, cleaning and cooking in her household, with a man whose social role is to be served by this woman?
The complexity of this clinical diagnosis is why I cannot answer one of the most seemingly simple questions: are women at higher risk for dementia than men?
Dementia is a loss of memory and thinking that affects someone’s ability to function in everyday life. Dementia isn’t a disease itself, it’s caused by other diseases, such as Alzheimer’s, vascular dementia, Lewy body dementia, alcohol use disorder and others. Deter had a rare genetic cause for her dementia, but for most people dementia is not a strictly genetic disease, it’s related to lifestyle and factors that we don’t yet understand. Even more, once people are over 80, very few have pure Alzheimer’s pathology. Damage to blood vessels become more strongly associated with cognitive decline than the build-up of amyloid plaques.
I can diagnose diabetes based on a number on a blood test: it is binary and quantifiable. When I diagnose dementia, it’s based on my subjective judgment that the person’s cognition has declined to the point that they can no longer fulfil their social role. I make this judgment based on a history from someone who knows the patient well, cognitive testing, blood tests and brain imaging, largely to rule out other causes. It’s not binary, it’s not completely quantifiable. This clinical diagnosis means that it’s possible that two different clinicians could see the same patient and come to a different conclusion about whether or not they have dementia.
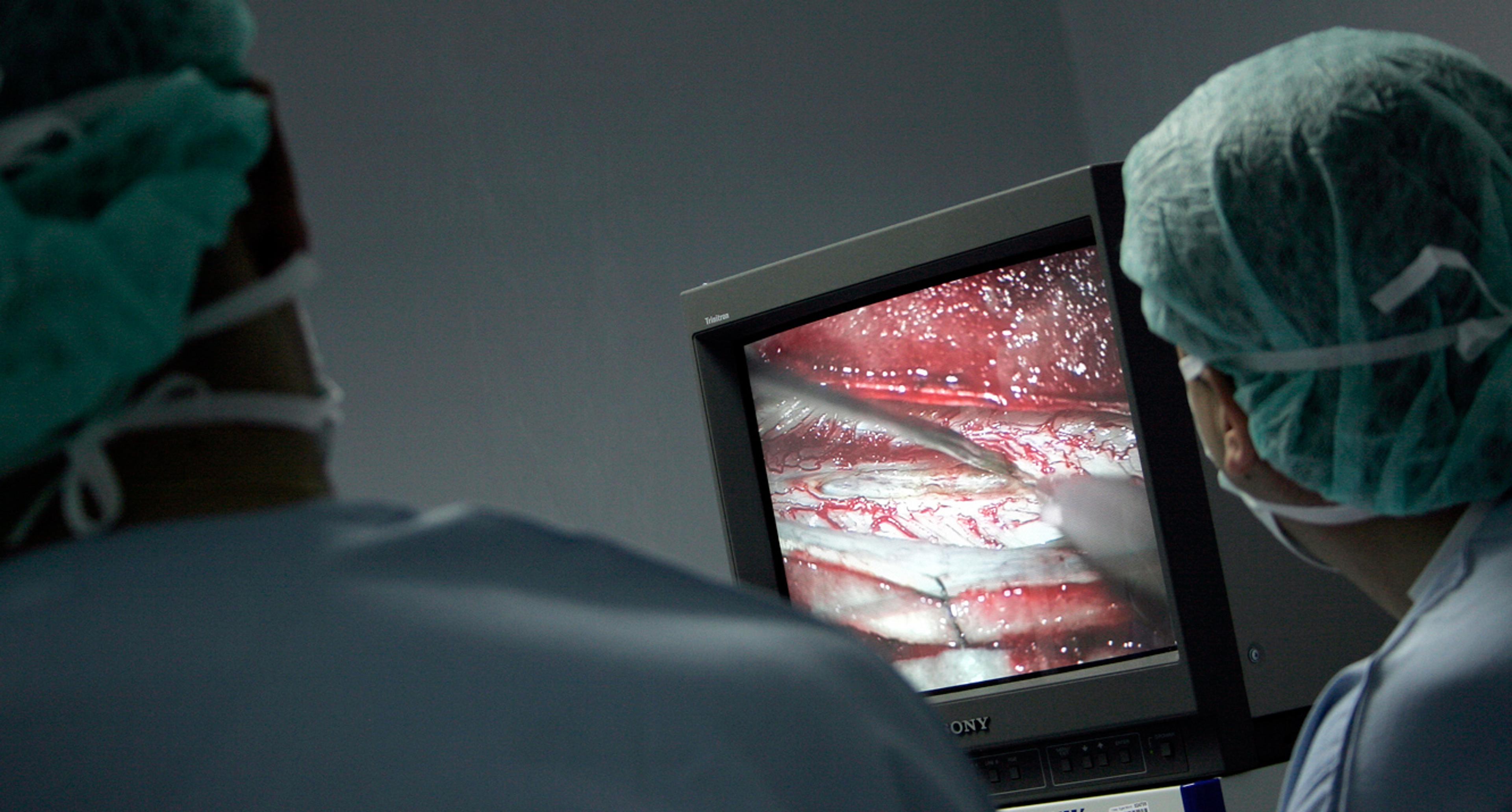
The only way to definitively diagnose which disease is causing the dementia is with a post-mortem examination. Clinically, late dementia is easy to identify: the decline in cognition means that the disability is significant, and is accompanied by a history of slow progressive decline over years. The early stages of dementia are much more subtle and varied, and there is less agreement between clinicians. In one study, researchers asked four experienced clinicians to review case notes for 40 people from their first clinical encounter through to their subsequent death from a pathologically confirmed diagnosis of dementia. The clinicians were asked to use defined clinical criteria. For Alzheimer’s, there was agreement between the majority of clinicians, but this was far from perfect. For people with a different type of dementia, Lewy body disease, agreement was very low.
Even though there are accepted criteria for diagnosis of different types of dementia, when I take a clinical history from a patient and their loved one, a standard set of questions isn’t enough. I need to learn about their life and how they spend their days, so I can find out what they no longer do. Given the influence of biological sex on gender, this can mean asking very different question for men and women.
Sex refers to biological sex: it is usually defined by whether an individual has two XX chromosomes or an X and a Y chromosome. Gender is a cultural construct that men and women have defined social roles based on these biological attributes. When an embryo has developed into a baby and is pronounced a boy or a girl, the social construct of gender takes place as they learn what their society decrees are masculine and feminine traits. From the time of birth, it’s hard to unpack sex and gender, particularly since biological sex is strongly associated with gender. While gender identity exists along a spectrum, for this article, I will be treating it as a binary, because for the life course of many older adults, this was the only socially accepted option.
Some people have argued that women are at a higher risk of dementia because, on average, men have larger brains than women, but this crude argument rapidly falls down because men are not more intelligent than women. While men do have bigger brains, on average and accounting for body size, women have a thicker cerebral cortex – the outer layer of the brain responsible for interpreting sensation, as well as higher cognitive abilities. These differences are subtle, and it’s impossible to look at an MRI of a brain and determine whether it’s from a man or a woman.
Though there are no differences in intellectual capacity, for so many of my patients, from childhood onwards, their social role has been defined by gender, from educational opportunities to work, childbearing and the authority within their own household. These things and many more all influence the development of dementia and the way that dementia is diagnosed.
One seemingly simple question we don’t know the answer to is how many people are actually living with dementia and how many are women; because around 50 per cent of people living with dementia are undiagnosed, all we have are estimates.
A study published in 2013, based on other longitudinal studies, estimated that there are 4.7 million people aged over 65 living with dementia in the United States, and others have estimated that two-thirds of these are women. This number was calculated by extrapolating the prospective Chicago Health and Aging Project (CHAP), where a cohort of almost 4,000 people had repeated cognitive assessments, to the US population. The estimate that two-thirds of people with dementia are women was made despite the original cohort in Chicago having no difference in rates of dementia diagnosis between men and women.
This is even more complicated if we look at historical cohorts. Older studies of gender and prevalence identified dementia as being more common in women. In a meta-analysis published in 1999, women over 85 had a far higher risk of being diagnosed with dementia than men. Within this meta-analysis there were significant differences between countries: in the US there was no difference between the sexes, but women in Europe and Asia were at higher risk. The studies used a variety of methodologies to identify people at risk of dementia, including a screening test called the mini-mental state examination (MMSE), which is heavily influenced by education level. Since women have traditionally had lower levels of education and the study didn’t adjust for this, were these women more likely to have dementia, or were they just bad at the test?
While dementia is not a normal part of ageing, the biggest risk for getting dementia is simply getting older, and since, worldwide, women have a longer life expectancy than men, ranging from 10 extra years in Russia to half a year in Bhutan, more women reach their 80s and 90s when dementia risk rises. Women do have certain biological advantages that explain this improved life expectancy. Since the X chromosome contains many genes that are involved in immunity, women are more resistant to infections than men. The downside to this is that women are more likely to develop autoimmune disease. Women tend to live longer, but with more chronic diseases and higher levels of disability in older age, as though better able to survive physical challenges – and this is also true of dementia. Since the leading cause of death for men in the UK and Australia is ischaemic heart disease, perhaps men are also dying too soon to be diagnosed with dementia.
In a study of people who attended a memory clinic for a dementia diagnosis and then donated their brains in death, men had a lower level of pathology and a shorter time to death after diagnosis. It’s not clear from this study whether men died of dementia or not, but if fewer men live to older age, and men survive fewer years with dementia, that goes a long way to explaining why most people living with dementia are women.
‘Atypical’, when it refers to differences between genders, is problematic as it defines one group as the norm
The sex hormones also have a role in brain health, with oestrogen having a positive effect on brain function. Oestrogen helps women prepare for motherhood: during pregnancy, women’s brains become more plastic and more able to learn, ready for the challenge of parenting a newborn.
Many women in mid-life experience brain fog, or functional cognitive disorder, especially trouble with concentration and memory. Some women do experience a decline in memory and processing speed during the time of menopause, but these changes resolve once the hormonal changes have settled. It’s also a risky assumption to attribute ‘brain fog’ to hormones alone. Menopause can negatively impact sleep, which impacts cognitive function, and is also a risky time for the onset of depression. So many women who experience this brain fog are terrified that this is the start of dementia, but there’s no evidence that it’s the start of an inexorable decline.
This also brings up one of the most challenging aspects of studying dementia: to understand a disease that takes decades to develop, we need decades-long research studies, and these are expensive and difficult to do. To understand whether the fog of menopause is truly a risk for dementia, we need studies that run for four to five decades, and include men and women.
While we don’t have the evidence to link brain fog to dementia, we do know that an early dip in oestrogen from oophorectomy (removal of the ovaries) is a risk factor for the development of dementia, as is an earlier onset of menopause. This might or might not be purely the effect of the oestrogen on the brain because, when women lose the protective effects of oestrogen on cardiovascular health, this can also impact the health of the blood vessels in the brain.
One common misconception about dementia is that it’s purely forgetting. The decline in cognitive function can impact any domain, like an art historian I saw who had damage to the occipital lobe of the brain, which interprets visual information and so could no longer identify paintings. Some get marked language impairment early, still able to follow well-known processes, but not able to find the words to name common objects and people. Other people can become apathetic, able to perform well on simple memory tests, but with no drive at all to undertake personal care. Some develop personality change, becoming labile and easily irritated.
The initial forgetting in dementia usually manifests first as an inability to remember new information. This kind of amnesiac forgetting means that the new information is instantly gone, but the memories of a lifetime are usually retained early in the disease. Men are more likely to present with ‘atypical’ symptoms, less forgetting and more behavioural disturbance and apathy. The term ‘atypical’, particularly when it refers to differences between genders, is problematic because it defines one group as the norm. Women are less likely to be diagnosed with heart disease because their symptoms are less likely to fit the defined norm of chest pain. If men are less likely to have forgetting as an early symptom, perhaps they’re just not getting diagnosed with the dementia they have?
One risk factor that’s more common in women than men is depression, but this risk factor is also a mimic. People who are depressed can have slowed cognitive processing, lack of initiation and interest, and poorer memory, especially for new things, all common symptoms of dementia. When someone comes to see me because they’re worried about their memory, it can be incredibly difficult to work out whether it’s a mood disorder or the beginnings of dementia and sometimes only time and treatment will tell. People with depression can also have shrinkage in the hippocampus, a critical structure for memory, so treating depression in midlife might be a key strategy for reducing rates of dementia.
To diagnose dementia, the most important information is taking a history from someone who knows the patient well, to get the story of a slow, progressive decline in cognition; also, asking about what the person likes to do and whether they have lost certain skills and abilities. Many people with dementia forget that they are forgetting or lose insight into their decline – so, without a concerned advocate, they go undiagnosed.
I once saw a man who scored 3 out of 30 on his cognitive screening test, with a wife and daughter who initially denied that there were any problems with his memory. This man spent his days walking his dog around his local streets (or perhaps the dog was walking him); his wife did everything else for him. His role in the family was to be served by women, so the family had simply continued to serve him. I see whole families who have rearranged their lives around a man with advanced dementia, ensuring that he’s constantly supported, helping him wash and eat, without ever seeking a formal diagnosis. Perhaps it’s my own bias that I remember more men than women where this has happened.
I see women, often those married their entire adult life, who will deny, even when it seems so obvious to me, that their husband has dementia. I wonder if admitting cognitive frailty undermines his masculinity in a way that’s unfathomable, after a lifetime structured around the idea that a man is the leader of the house.
Since diagnosis of dementia depends so much on subjective opinion, sometimes of a multidisciplinary group, how can individual clinicians ensure that we’re not bringing our own bias to the consulting room? When I diagnose someone with dementia, I’m predicting an inexorable loss of that person’s abilities. I am telling them that their memory will become fitful and faulty, first losing the ability to retain new information, then gradually losing their own biography and knowledge of their identity. Late in the disease, they will lose the ability to walk, then to chew food and swallow. I must tell them that there’s no treatment that will stop the progression of this terminal neurological disease.
The end stages of dementia are undeniable. But the moment when someone transitions from ‘not disease’ to ‘disease’, from being ‘normal’ to having the label of a degenerative neurological disease, isn’t a clear inflection. Often, it’s only in hindsight that it becomes obvious just how long the disease has been developing; the partner of one man I diagnosed told me that, in hindsight, the decline began eight years earlier, when he stopped making art.
When I speak to patients through an interpreter, I feel as though we’re speaking through a haze
When the moment of inflection and diagnosis is influenced by a lifetime of experience, how do we standardise people in a drug trial, especially when gender is involved?
I use the concept of gender as a binary construct, but of course, it’s not. Two people who identify as women can have vastly different life experiences. My own grandmother grew up in Australia in a very middle-class family, finished school, completed education and held a professional job outside the home. I see other women her age who were born overseas into poverty, who had three years of formal education interrupted by war, women who migrated to Australia and worked in factories with others who spoke their first language, never having the opportunity to learn English, women who have had a life experience that I can’t even imagine. When I speak to patients through an interpreter, I feel as though we’re speaking through a haze.
And understanding dementia as a life-course disease makes it even harder to apply information from past research to the future. Women’s education levels are changing, with more than ever graduating from university. So can we really apply knowledge gained from people in their 80s and 90s now to people currently in their 20s and 30s? Can we confidently quote studies from 30 years ago that found higher rates of dementia in women, when those women had less educational opportunity and most likely worked within the home?
At a certain level, every disease is an artificial construct. We categorise bodily functions to ‘normal’ and ‘not normal’, as if there is a chasm between the two states instead of a steady slope connecting them. For some of my patients, hallucinations of deceased loved ones is a sign of illness, for others it’s culturally appropriate. Even the definition of diabetes, a defined cut-off on a blood test, is arbitrary: the person with a fasting blood sugar of 7.1 is not so different from the person with a blood sugar of 6.9, but one has the label of disease, and the other doesn’t.
Like Alois Alzheimer, I record symptoms, conduct tests and assign the label of disease. For a patient with dementia, I can assign this label based only on my subjective opinion, and only after finding out more about a trajectory of decline from someone who knows the patient well. Both their impression and mine merge to determine whether someone can no longer fulfil their role. While clinicians do try to account for education, lifetime occupation, family circumstances, culture and gender, our adjustments are imperfect.
It seems like a simple question to answer whether women are at a higher risk for dementia than men, but I cannot. We need longer duration studies that actively account for gender, life experiences and age. We also need to validate biomarkers to help standardise the diagnosis. Maybe then, there will be a time when I can give my patients both a diagnosis and a cure.
To read more about ageing and memory, visit Psyche, a digital magazine from Aeon that illuminates the human condition through psychology, philosophical understanding and the arts.