Most health-conscious people are familiar with the concept of risk factors for disease. We’re too familiar, in fact. A risk factor is like the guest that nobody invited to the party, a spoiler. Though we might feel fine now, our individual risk for (fill in the blank) tells us that our wellbeing might not last. That vague and remote prospect of a stroke or a tumour has taken on a sharply numerical precision, thanks to screening tests that expose and quantify our risk factors.
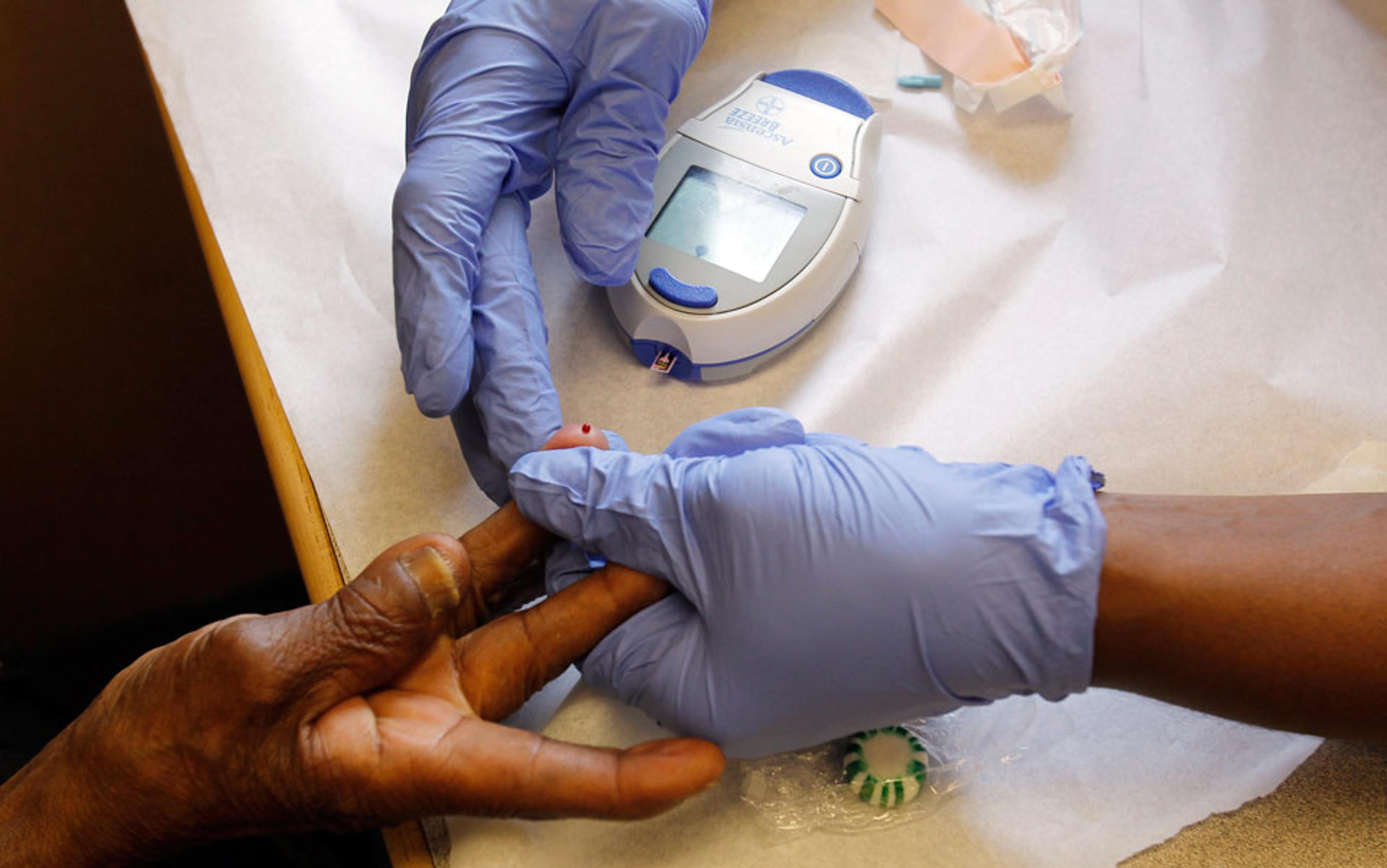
The term stems from the Framingham Heart Study, which began in 1948. Ever since, researchers have measured the variables that contribute to cardiovascular disease in multiple generations of residents of the town of Framingham in Massachusetts. The participants did not have cardiovascular disease when they enrolled, but researchers routinely recorded factors suspected in disease onset, including blood pressure, cholesterol levels, and whether or not the person smoked.
Since no single factor was able to predict the heart attacks that occurred in Framingham, the study designers thought to combine half a dozen of them in what became the first numerical risk calculator, called the Framingham Risk Score. The researchers figured the relative importance of each risk factor after examining thousands of health histories. The combined risk score enabled doctors to make predictions that were borne out in future patients as the study proceeded.
Dozens of risk calculators are in service today, covering all medical specialties and organ systems. But since Framingham, risk factors have acquired an unwarranted power. Doctors try to manage them as if they’re the disease itself and, as a result, patients are subjected not only to undue worry but also to the harmful side effects of preventive medications and testing.
What’s more, in medicine’s version of mission-creep, the thresholds for many risk factors have been lowered so as to encompass ever larger pools of patients. People who believed they were normal in a particular health category abruptly learn that they are not – and that they probably need treatment. That they lack symptoms is misleading. Today’s patient is declared to be in good health not because she feels well, but because her latest scan or blood work indicates no abnormalities.
Robert Aronowitz, a historian of medicine and medical doctor at the University of Pennsylvania, points out that when drug companies are able to treat people who might become sick, as opposed to patients with symptoms, the market is a lot larger. Once put into the at-risk category, they might be taking medication for the rest of their lives. Aronowitz gives hypertension (high blood pressure) as an example: a risk factor for heart disease and stroke, it makes the arteries more prone to blockage and rupture. The first drugs developed for hypertension were used to treat people showing obvious signs of spiking pressure, such as shortness of breath and nosebleeds. Next, the medications were extended to people without symptoms who nonetheless had hypertension upon measurement – a systolic pressure (when the heart is pumping) of above 140, and a diastolic pressure (when the heart is at rest) of above 90. These patients, a much larger population, numbering in the tens of millions, had to be screened to be identified.
The threshold of what constituted a safe level of blood pressure ‘was gradually lowered’, writes Aronowitz. ‘And finally a new disorder, prehypertension, was defined and promoted, such that another segment of the population could be screened, labelled, and treated.’ ‘Prehypertension’ represents a systolic pressure of between 120 and 140, and a diastolic pressure of 80 to 90. Those ranges used to be considered normal, but not anymore.
Recently, the American Heart Association (AHA) recognised that things had gone too far. Since studies had shown that blood-pressure medication was of no benefit to those with prehypertension, the AHA raised the level at which people aged 60 and over should start taking drugs. Now the recommended trigger is a systolic pressure of 150 or higher. With the change, some 7 million Americans, more than half of whom were taking medication, were moved out of the at-risk column. It’s unlikely that 3‑4 million people will drop their medications, however. Once launched, a medical regimen of that magnitude is hard to turn around.
There’s a more fundamental issue. Risk factors and risk calculators are reminders that medical science does not completely understand the mechanisms of disease. Risk factors are associations; they don’t represent cause-and-effect relationships unless the connection to the disease is especially strong, like the link between cigarettes and lung cancer. Risk factors are based on averages taken from large groups, and consequently the individual patient can’t know his or her true probability of contracting the condition. For any population, the calculator could accurately forecast the number of, say, heart attacks over a 10-year period, but the algorithm can’t identify who will succumb and who will be spared.
Thus the AHA, in releasing its latest risk calculator for heart attack and stroke, admitted that ‘no one has 10 per cent or 20 per cent of a heart attack during a 10-year period. Individuals with the same estimated risk will either have or not have the event of interest, and only those patients who are destined to have an event can have their event prevented by therapy.’ Which is to say that the majority of patients are going to dodge a bullet whether or not they use preventive therapy. The doctors, for their part, plead that they are only being conservative. Unsure of the basic biology of the disease, they overtreat the many in order to help the few.
What’s the harm in this? Well, no medication is free, nor is it exempt from complications and side effects. Take statins, the blockbuster drugs used to lower low density lipoproteins (LDL) or ‘bad’ cholesterol. Statins are a $30 billion market worldwide. In the US alone, a quarter of those aged 40 and over take them to control a major risk factor for heart disease. Statins have succeeded in reducing both LDL cholesterol and deaths, but cardiologists have belatedly recognised that their preventive strategy was arbitrary. Patients were told to strive for a LDL target of 70 milligrams per deciliter, when there was no evidence that such a drastic reduction would prevent heart attacks and strokes. Less extreme reductions should work as well. Lisa Schwartz, a community medicine expert at the Dartmouth Institute for Health Policy and Clinical Practice, says: ‘Selling statins was about lowering cholesterol when it should be about managing heart-attack risk.’ In other words, because it was amenable to measurement and manipulation, the risk factor became the therapeutic object and diverted attention from the complexity of cardiovascular disease.
In November 2013, the AHA and the American College of Cardiology (ACC) abandoned specific LDL targets in calculating the need for statins. Instead, the professionals recommended the drugs for four categories of patients. The first three were obviously at risk: diabetics; those already suffering from heart disease; and those with very high LDL, who might lower it with statins without having to meet a particular benchmark.
In the fourth category, by far the most controversial, were people who should take statins because they ‘flunked’ the new AHA/ACC risk calculator. Specifically, these were people whose risk factors produced a 7.5 per cent or more chance of a heart attack or stroke over the next 10 years. According to one estimate, the new AHA/ACC guidelines would add almost 13 million people to the US population of potential statin users, a total of 56 million people. Anybody over 60 was virtually guaranteed to qualify because his or her risk of heart attack and stroke was already elevated due to age. Although the calculator looked to have been designed by the drug companies, it was an updated version of the original Framingham Risk Score, and the AHA and the ACC defended it stoutly.
my health was excellent but the computation told me that my risk of heart attack or stroke was above the trigger point
So I put myself to the test, entering my information in the calculator online. The nine variables were my age, sex, race, total cholesterol, HDL (high-density lipoproteins, or ‘good’) cholesterol, systolic blood pressure, blood pressure medication (yes or no), diabetes (yes or no), and smoking (yes or no). I couldn’t help my age (67) , but the rest of my profile was good. My blood pressure and cholesterol were relatively low. I don’t smoke or have diabetes. So far as I knew, my health was excellent. The computation told me that my risk of heart attack or stroke was 15.3 per cent, or above the trigger point. Therefore I was invited to discuss statin therapy with my doctor.
This I declined to do, fortified by another calculation. It took some digging to get the numbers but, according to experts, statins would lower my risk by only four percentage points, from 15 to 11 per cent. Here’s how to visualise the math. Imagine 100 people like me: white men aged 67, with identical blood pressure (125) and cholesterol values (total 184, HDL 39). No cigarettes, diabetes, or antihypertensive drugs in the group. The AHA/ACC calculator predicts that 15 of us will suffer a nasty cardiovascular event within a decade.
Now let’s give statins to all 100 of the group over a 10-year period. Right off, five of us will have muscle pain as an unavoidable side effect. (Statins are also reported to have caused cognitive and psychiatric problems in some individuals.) Of the 15 subjects who were slated to have a heart attack or stroke, just four are spared by the statins, leaving 11 men who were stricken in spite of having taken medication and 85 others who would have been all right had they not taken medication. The bottom line is that doctors have overtreated 85 people in order to protect four. If statins could eliminate my cardio risk entirely, that would be one thing, but to lower it by four percentage points, when it wasn’t high to begin with – no, I’d rather bet that I’m one of the fortunate 85.
Risk factors and risk calculators are the drivers of what Aronowitz calls the screen-and-treat paradigm. Population screening funnels large batches of patients through blood tests and scans, and a minority emerges with early warning signs of disease and advice for combating them. The focus on early detection is one reason that the US has the most expensive medical system in the world. The effort might be worth it if screening tests never had false positives – if they uncovered only those conditions that needed to be uncovered. But as medical technology has become more sophisticated, so has the detection of benign masses and ambiguous blood values, which become the grist for overdiagnosis and costly overtreatment.
Similar to overtreatment, overdiagnosis refers to the identification and labelling of conditions that aren’t going to matter clinically. For example, many researchers have found that mammograms detect tiny, harmless masses or unthreatening ductal carcinomas in situ (DCIS), leading to thousands of dubious treatments for ‘cancer’ per year. In 2012 a study by the oncologist Gilbert Welch and the internist Archie Bleyer in the New England Journal of Medicine estimated that breast cancer had been overdiagnosed in 1.3 million women in the US in the past 30 years, about one‑third of the total cases. The oncologist Laura Esserman of the University of California at San Francisco has led a campaign to strip the word carcinoma from DCIS. It’s not cancer, she says. Esserman’s view is that women might not feel as compelled to choose aggressive, immediate treatments if the condition were properly labelled.
for every life saved, three women had preventive treatments that they didn’t need
Because of population screening, the prevalence of breast cancer has gone up sharply since the late 1970s, but the increase consists mainly of early stage cancers and DCIS. The number of late-stage cases has been only marginally reduced, if at all. This means that catching and treating DCIS hasn’t blunted the appearance of serious disease.
The party line holds that mammography saves lives, but the benefit is much smaller than most women know, about one life for every 1,000 women who are screened regularly after 50. Without mammography, there are five deaths per 1,000 from breast cancer; with it, four. To save that one extra life is important but, to achieve it, hundreds of women pay a price in unnecessary biopsies, treatment, radiation exposure and distress. According to a study this spring in the Journal of the American Medical Association, having an annual mammogram for 10 years results in a 60 per cent chance of a false positive and a 20 per cent chance of an overdiagnosed tumour. A 2012 review of mammography in the British journal The Lancet concluded that, for every life saved, three women had preventive treatments that they didn’t need. These are harms that ought to be avoided.
To be fair, it is asking a lot of a screening programme to tell the difference between an indolent cancer that will not progress and an aggressive one. Of the major types of cancer, only colon cancer is well-suited to the screen-and-treat paradigm. Slow to develop, colon cancer is preceded by a reliable risk factor – polyps. When these are snipped off during colonoscopy screening, the disease is stopped in its tracks.
About eight years ago, after two of my brothers had cancerous prostate glands removed, I grew concerned about my own cancer risk. My doctor had two ways to screen my prostate for a tumour: the digital rectal exam, whereby he felt around for a nodule or enlargement, and the PSA test, for prostate-specific antigen, a marker measurable in blood, which was meant to take the guesswork out of the digital exam. Averaging 230,000 new cases a year, prostate cancer had become the most commonly diagnosed cancer in the US, not counting skin cancers, and the PSA test was the reason.
Although there was no research then to show that PSA screening actually saved lives, the test had become de rigueur for middle-aged men, such was the desire to have something – anything – to use against prostate cancer. Now the evidence has come in. In two major trials of PSA’s effectiveness, scientists followed two groups of men over time, one group getting PSA screening and the other not. There was almost no difference in mortality between the groups. At best, the screening programmes prevented one death per 1,000 participants.
As a risk factor, PSA is very unreliable. Whether or not cancer is present is determined by a painful biopsy and, according to statistics, only a quarter of biopsies performed each year are positive. But if cancer is detected, the patient feels tremendous pressure to have it out, notwithstanding that indolent prostate tumours far exceed the aggressive ones. Autopsies of men in their 80s who die of other causes show that 70 per cent of them have cancerous prostates, but while they were alive they never had symptoms. Certainly surgery can eliminate the cancer whatever its grade, but grievous side effects such as incontinence and impotence are almost as certain to follow.
Some of this I knew then, some I didn’t. My PSA had been climbing, albeit slowly. Hesitating at the entrance of the screen-and-treat maze, I decided to take a second PSA test a few weeks after the first in hopes of achieving a lower score. The level dropped a little, which was an artifact either of the laboratory or my hormones. My doctor still thought it was high enough to warrant a trip to the urologist.
After examining me, the urologist ran my medical information through his risk calculator for prostate cancer. The inputs were my family history (yes, I had relatives with prostate cancer), age (at the time I was 59), race (white), and PSA level (2.9). Also included were the urologist’s digital rectal exam result (normal), and whether I’d ever had a negative biopsy in the past (no, since I’d never had a biopsy before). Crunching the information, the calculator estimated that if I underwent a biopsy today the chance of it being positive was 35 per cent. That was a bit higher than average.
The risk calculator spat out one more figure for me: the probability that a biopsy would detect a high-grade, fast-growing tumour, the one to be feared. The risk of that was only four per cent. I breathed easier and pushed a biopsy from my mind. Thereafter, I didn’t worry so much about the PSA readings on my annual blood work. PSA naturally goes up with age, I reminded myself.
In 2011, I stopped PSA testing altogether, and the next year the US Preventive Services Task Force, an independent medical body, came out against screening, saying that, on balance, it led to more harm – including psychological – than good. Urologists have responded by ordering fewer tests in younger men, but PSA screening, though flawed, will persist as long as some men won’t tolerate the possibility of harbouring a tumour. Until a better test is devised, PSA will continue to trigger a diagnostic cascade ending in unnecessary prostate surgeries and radiation. Personally, I am willing to accept a small chance of dying to avoid the harms of overdiagnosis and overtreatment.
When I told Aronowitz that I’d dropped out of PSA testing, blinding myself to my risks, he said: ‘I’m pessimistic that medical consumers can resist being “saved”, but yes, some degree of dropping out is necessary. We need to have a conversation about how to make people more skeptical.’ Sometimes we should educate ourselves just enough to say no.
Hypnotised by the swings in relative risk factors, we might miss the more hopeful numbers surrounding absolute risk
If there is one lesson the medical consumer ought to master, it is the difference between absolute risk and relative risk. Health journalists are constantly reporting relative risks – how medication X lowered the risk of health outcome Z in a group of patients, compared with a similar group that didn’t take X and had a higher rate of Z.
Let’s assume that the drug X achieved a relative risk reduction of 50 per cent. That sounds impressive until you read, probably not in the article but in the fine print of a medical journal, that the prevalence of Z, the absolute risk to everyone in the study, is only two per cent. Thus the pill has cut the actual risk from two per cent to one per cent. In light of that slender benefit, X’s side effects and price tag loom large. Risk factors for disease are also relative entities, having been derived from a comparison of patients, one group healthier than another. Hypnotised by the swings in relative risk factors, we might miss the more hopeful numbers surrounding absolute risk.
Ultimately, what we really want to know is our risk of death. Just as risk factors are painless proxies for the threat of disease, so worries about disease substitute for fears about dying. I know that my death creeps closer with each passing decade, but I manage my mortality by fractionating the absolute risks of death’s vehicles. As noted, my risk of a heart attack or stroke is 15 per cent, though the odds that either would be fatal are far lower. My lifetime risk of dying of prostate cancer is just one in 38. Because of family history, I’m going to bump it up to one in 30, still a low probability, nothing to lose sleep over.
According to the statistics, no other cancer out there is more likely to kill me than prostate cancer. You see how it works? Someone might inconveniently point out that invasive cancer as a whole has a one-in-four chance of getting me, but I’m not listening to that someone. As Schwartz says: ‘Bad things don’t happen that often. To go from an eight per cent to a seven per cent death reduction is important to doctors, but it may not be to individuals. Do you want to take a pill every day to reduce a small risk?’
I don’t.