‘I am too young to die,’ said my patient. ‘My kids are small. They still need me.’ I explained that having a heart attack did not mean that she would die. We had caught it early. Within the next minutes, she would have an angiogram to remove the blood clot in her coronary artery, and we had already started her on a nitroglycerine drip and an infusion with a blood thinner. But I understood her fear. Women in their early 40s and in good health are not supposed to have heart attacks. She was not overweight, she never smoked, she had no history of high blood pressure or high cholesterol, and nobody in her family had ever had any heart problems. As we wheeled her away, she said that her chest pain was easing up. She was trying to be brave, but I could still see tears in her eyes.
Twenty minutes later, the interventional cardiologist and I stared at the angiogram images. My eyes kept flicking back to the electrocardiogram that had prompted our diagnosis. It had indicated the presence of a clot blocking an artery of the heart, but the angiogram showed completely pristine arteries: no clot, no plaque. I gave my patient the good news and saw her smile and utter a prayer.
Over the course of the next 24 hours, blood tests confirmed that she’d suffered a heart attack. Perhaps she had an exceedingly rare condition in which transient spasms of coronary arteries can cause a heart attack. Perhaps there had been a clot in her artery but it had dissolved before the angiogram, thanks to the intravenous blood thinner. The blood tests and ultrasound images showed that the damage to the heart was minimal, probably because the blood flow had normalised so quickly. I was happy for her and her family, but I was bothered by a nagging question. Why would a young, healthy woman with normal coronary arteries suffer a major heart attack?
She was taking one regular prescription medication: an oral contraceptive. One of its rare but significant side effects is the increased rate of blood-clot formation. The risk varies from one pill to another, but can be twice, threefold or even higher for oral contraceptive users when compared with women who do not use them. The risks are still small: a recent study monitored 1.6 million women in Denmark (ages 15-49) over a 15-year duration, and found that only 3,311 women had a stroke related to a blood-clot formation, and 1,725 women had a heart attack. My patient was using an oral contraceptive for which multiple studies had confirmed an association with blood-clot formation.
In clinical practice, it is often very difficult to prove cause and effect. Diagnoses are derived from the recognition of correlations or patterns, and frequently based on educated guesses instead of definitive scientific evidence. In this case, we advised our patient to stop using oral contraceptives. She recovered completely, and has had no recurrence of a blood clot or other major health problems. We will probably never know for sure whether contraceptive pills contributed to her heart attack, but her case serves as an important reminder that these risks are real.
The arrival of the birth control pill in the 1960s was hailed as a social revolution that decoupled sexuality from reproduction. It empowered women by giving them true reproductive control, because it allowed for reliable and reversible contraception. Women could delay or prevent reproduction without having to abstain from sex, and they could discontinue usage if they wanted to have a child. Over the years, many additional female contraceptives have been developed so that women today can choose from pills, injections, patches or intrauterine devices — many of which are even more reliable than those of the 1960s.
By contrast, the choices for male contraception are far more limited: it’s either sterilisation (a vasectomy) or condoms. Vasectomy has been used since the late 19th century, while the condom has an even longer linage. In the 16th century, the Italian anatomist Gabriello Fallopio described a condom made out of a linen sheath, used to prevent the transmission of syphilis. By the 18th century, condoms were prized as male contraceptives, and were even mentioned by the Italian adventurer Giacomo Casanova, who described them as ‘English Overcoats’.
Condoms can prevent the spread of sexually transmitted diseases, but, as a reproductive control strategy, they are not as reliable as their packaging suggests. Unintended pregnancies occur in up to 18 per cent of couples who rely on condoms for contraception. Vasectomies are very effective, with less than a one per cent ‘failure rate’, but they are extremely difficult to reverse. A change of mind means complex microsurgery with uncertain results. In a society that increasingly recognises that men and women should share responsibilities and opportunities equitably, the lack of adequate reproductive control methods for men is striking — and puzzling — especially since many newer methods for male contraception have been developed during the past decades yet none has become available for general use.
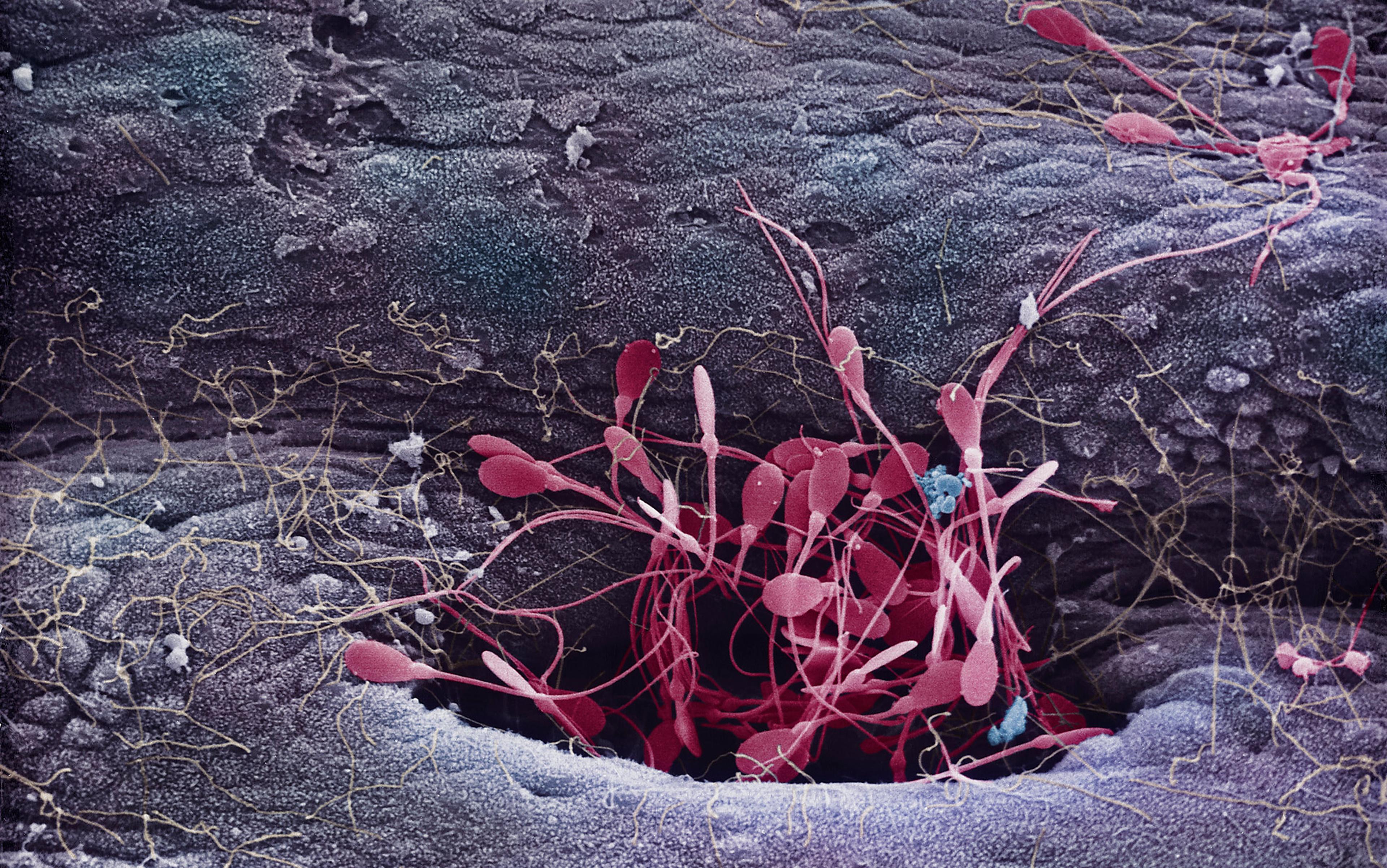
Newer approaches to male contraception can be divided into two groups: hormonal and non-hormonal. Hormonal male contraceptives act by reducing testosterone levels in the testicles, which drive the production of sperm cells. Most hormonal male contraceptives that have been studied in clinical trials involve the administration of testosterone, either as an injection, implant, oral pill or patch. It might seem counterintuitive to supply extra testosterone in order to suppress sperm-cell production, but this approach works by taking advantage of an internal brake in the male reproductive system. Testosterone production in the testicles is activated by hormones released from the pituitary gland of the brain — the follicle-stimulating hormone (FSH) and the luteinising hormone (LH). Some of this testosterone seeps out from the testicles into the bloodstream and signals to the brain: ‘Stop releasing FSH and LH, there is more than enough testosterone to go around!’
A testosterone-containing contraceptive mimics this function by increasing testosterone levels in the bloodstream, thus activating the shutdown signal. The brain responds by turning off the FSH and LH production; the testicles stop making their own testosterone. Testosterone levels in the testicles start to ebb, eventually dropping below the threshold required for adequate sperm-cell production. The levels of testosterone in the bloodstream supplied by the contraceptive are sufficient to maintain masculine features and male libido, but cannot compensate for the loss of testosterone in the testicles, and thus cannot restore sperm-cell production. Newer-generation male hormonal contraceptives combine testosterone with another class of synthetic hormones called progestins, also used in female contraceptives and extremely effective at activating the FSH/LH shutdown.
So far, clinical trials have shown that it takes time — six weeks or longer — until sperm counts drop low enough to stop fertilisation. Short-term studies of the side effects of male contraceptives have not revealed anything major: acne, weight gain, increased libido. Most male contraceptive trials have been small, often recruiting only 10-100 men, and the measured ‘success’ was based on achieving undetectable or minimal sperm counts. Yet the ultimate test of efficacy is not a drop in sperm counts but the prevention of unintended pregnancies in couples who rely on these contraceptives as their primary method of reproductive control. Such efficacy trials require the recruitment of a large number of volunteers and their costly long-term monitoring. Large-scale studies are also needed to ascertain the long-term safety profile of male hormonal contraceptives.
‘None of the big companies will touch hormonal male contraception again’
One of the largest male contraceptive efficacy trials ever conducted was sponsored by the World Health Organisation (WHO) and CONRAD, the US-based reproductive health research organisation. Called Phase II TU/NET-EN, this landmark multicentre study was designed to answer key questions about the long-term safety and efficacy of male hormonal contraception, and enrolled more than 200 couples between 2008 and 2010. The contraceptive used was a long-acting formulation of testosterone (testosterone undecanoate, or TU) combined with a long-acting progestin (norethisterone enanthate or NET-EN), administered via injections every two months. The trial included an initial treatment phase to suppress sperm production, and a subsequent ‘efficacy phase’ that required couples to rely exclusively on this form of birth control for one year. However, in April 2011, the trial was terminated prematurely when the advisory board noticed a higher than expected rate of depression, mood changes and increased sexual desire in the study volunteers. By the trial’s end, only 110 couples had completed the one-year efficacy phase; their efficacy results should be released in the near future.
The trial did not include a placebo control group, so the investigators could not determine whether the observed side effects were due to the hormone combination or a side effect of frequent injections. Just like we do not perform ‘placebo’ or sham surgeries on patients, we cannot in good conscience enrol people in a placebo group of a contraception efficacy trial, because most of the couples in the placebo group would end up with an unintended pregnancy.
The discontinuation of the WHO/CONRAD trial was a major setback in bringing male contraceptives to the market. It also raised difficult ethical questions about how to evaluate side effects in male contraceptive trials. Since all medications are bound to exhibit some side effects, what side effects should be sufficient to halt a trial? Female contraceptives have been associated with breakthrough bleeding, mood changes, increased risk of blood-clot formation, as well as other side effects. Why should we set a different bar for male contraceptives?
The twist here is that female contraceptives prevent unintended pregnancies in the person actually taking the contraceptive. Since a pregnancy can cause some women significant health problems, the risk of contraceptive side effects can be offset by the benefit of avoiding an unintended pregnancy. However, men do not directly experience any of the health risks of pregnancy — their female partners do. Thus it becomes more difficult, ethically, to justify the side effects of hormonal contraceptives in men.
What of non-hormonal contraceptives for men? Instead of targeting the hormonal axis that connects the brain and the testicles, non-hormonal contraceptives act directly on the production, activity or movement of sperm cells. One such approach is known as a ‘chemical vasectomy’. Developed by Dr Sujoy Guha in India, RISUG (which stands for ‘reversible inhibition of sperm under guidance’) has already entered Phase III clinical trials. In a standard vasectomy, the vas deferens (the natural transport channels for sperm cells in the testicles) are cut and sealed so that sperm are unable to enter the seminal fluid. In RISUG, a synthetic polymer is injected into the vas deferens with the same effect, but with the dramatic benefit that this polymer can be removed during a further, simple procedure that should restore normal movement of the sperm cells.
RISUG is not without caveats. Unlike taking a pill or receiving an injection, it requires a small surgical procedure. And the data on RISUG reversibility is based on animal experiments. We do not yet know whether reversing it in humans would restore male fertility. The clinical trial data obtained in India has been very encouraging so far, both in terms of safety and efficacy. The non-profit Parsemus Foundation has obtained the rights to use and market the RISUG method in the US as Vasalgel, and intends to initiate the first US-based clinical trials this year or next. RISUG is probably unable to generate the kind of profits that would attract the attention of a pharmaceutical company: the synthetic polymer is inexpensive, and a single polymer injection is sufficient to suppress fertility for years. So the only hope for general availability is support from the non-profit or government sector.
Other non-hormonal contraceptive methods are currently under investigation in animal studies. Dolores Mruk and Chuen-yan Cheng, scientists at the Population Council in New York, have shown that the chemical Adjudin causes reversible infertility in animals by inducing the release of immature sperm cells. A collaboration between laboratories at Baylor College of Medicine in Houston and the Dana-Farber Cancer Institute in Boston showed that JQ-1, a small molecule that targets the epigenetic enzyme BRDT, was able to reversibly inhibit sperm-cell production and fertility in male mice. But these are a long way from availability. It might take five years or longer for additional safety and efficacy studies in animals before even a small pilot human study can be conducted.
If these hormonal and non-hormonal male contraceptives have been developed during the past decades, and some have been shown to be reasonably efficacious in small clinical trials, why are they not yet available for general use? Eberhard Nieschlag, professor at the University of Münster in Germany and a leading researcher in male fertility, recently described the impact of the suspension of the WHO/CONRAD efficacy trial on his field:
For male contraceptives to become approved for general use, more safety and efficacy data from larger clinical trials are required. The suspension of the WHO/CONRAD trial should have prompted an investigation into the scientific basis of the side effects, and could have led to a new trial with improved male hormonal contraceptives. But the pharmaceutical industry was not prepared to make that investment.
There is a multitude of reasons for the pharmaceutical industry’s reticence when it comes to male contraception. The efficacy and acceptability of female contraceptives sets a high competitive bar. The ethical problem of justifying potential side effects without any direct health benefits for men is another deterrent. And recent controversies related to the health insurance coverage of female contraceptives in the US underscore the even greater uncertainty of who would pay for male contraceptives if they were brought to market.
These investments make sense only if there is a large market for male contraceptives. Preliminary surveys seem promising: in 2000, Anna Glasier, professor of obstetrics and gynaecology at the University of Edinburgh, and her collaborators published an international survey of 1,894 women attending family planning clinics in Scotland, South Africa and China. Most women supported the idea of a ‘male pill’, and suggested that their partners would use it.
Newer male contraceptives require a very significant shift in the responsibility and burden of contraception between men and women
In 2005, a follow-up study by Klaas Heinemann at the Centre for Epidemiology and Health Research in Berlin surveyed more than 9,000 men in Europe, Asia, North America and South America. The willingness of respondents to use newer male contraceptives was highest in Spain (71 per cent), Germany (69 per cent), Mexico (65 per cent), Brazil (63 per cent) and Sweden (58 per cent). Nearly half of the men in the US (49 per cent) and France (47 per cent) expressed an interest. On the other hand, disapproval of newer male contraceptives was highest in Indonesia (34 per cent) and Argentina (42 per cent). These surveys reveal that there is a broad, international willingness among men and women to use male contraceptives, but such an endorsement of a hypothetical ‘male pill’ is a far cry from implementing it. To use newer male contraceptives would require a very significant shift in the responsibility and burden of contraception between men and women. We won’t know how that will work in practice until male contraceptives become widely available.
Scientific and cultural challenges might also explain the lacklustre involvement of the pharmaceutical industry. The efficacy data from small clinical trials has shown that there is significant biological heterogeneity in terms of how men respond to hormonal contraception. Suppression of sperm-cell production seems to be far more effective in Asian men, for example, than in Caucasian men. It is very likely that even within each ethnic group, there is a significant variability in the response to contraceptives. Instead of a ‘one pill fits all’ approach, male contraceptives might only be effective if individually tailored. The cultural challenge of introducing male contraception is also formidable. The Catholic Church strongly opposes all forms of contraception and, as the surveys have revealed, there is significant variation in men’s attitudes to male contraceptives.
It is thus not surprising that pharmaceutical companies are reluctant to invest millions in large-scale clinical trials. But without such trials, male contraceptives will not receive the regulatory approvals needed to bring them to market. We have reached an impasse. As a society, we recognise the importance of providing options for reproductive control, yet the responsibilities (and side effects) of effective contraception are carried largely by women. Men might never be able to share the physical burden of pregnancy, but they can share the responsibilities of child-rearing and contraception. If the market cannot support this, we need to find an alternative route.
Pharmaceutical companies make investment decisions based on profits, while non-profit organisations and government agencies have the luxury of supporting research that leads to equitable sharing — something that does not carry a defined monetary value. Non-profit organisations and government agencies are not in the business of manufacturing pharmaceuticals, but if they could conduct the larger clinical trials required and identify efficacious and safe male contraceptives, then the investment risk will be minimal for any interested pharmaceutical manufacturers, who could capitalise on the research to mass-produce and market the contraceptives.
Jump-starting the listless development of new male contraceptives will require a substantial amount of education and support. The Parsemus Foundation, the non-profit behind Vasalgel, and the Male Contraception Information Project, in San Francisco, have made a good start on the challenge by providing information about research on male contraceptives. Politicians need to be lobbied to ensure the adequate funding of government research agencies that specifically pursue the development of male contraceptives. There is also a place for public support: research studies are always looking for male volunteers, and non-profit organisations studying male contraception rely on donations. Male contraception is an excellent example of an opportunity for crowd-funding.
There has been a societal failure to produce a contraceptive method for men beyond the condom or the vasectomy, but now we have the chance to rectify that. Who will take the next step?
References and links to the research mentioned above are available here.