Human beings crave all sorts of things: coffee, sugar, sex, gambling, Xanax, porn, binge-watching TV shows, doomscrolling on social media, cocaine, online gaming, heroin, methamphetamines, hoarding. We each find different substances and activities alluring, and we develop distinct habits of choice. Cravings are an especially forceful and persuasive class of desires. When a craving strikes, it can be very tricky to resist or ignore. Sometimes we distract ourselves and move on with little effort. In other instances, it can feel nearly impossible not to act on a craving. What we’re drawn to, and what we’re vulnerable to, seems to reflect our individual personalities, preferences, cultural location, values, identities, coping mechanisms, and other life circumstances. So, why do we crave what we crave, and why are cravings sometimes so forcefully motivating?
One way to see the power of cravings is to think about substance addictions. Substance addictions present the sharpest example of how cravings seem to impact motivation and behaviour differently than other desires. Cravings make for one of the most challenging, baffling and terrifying aspects of addiction: no matter how devastating the consequences of ongoing drug use become for someone, as well as for those who love and care for them, no matter whether their addiction is no longer pleasurable, and no matter how adamantly they want and try to manage or stop their drug use, their attempts are continually overwhelmed by intensely motivating desires to engage in the addiction. This loss of control is often taken to be a defining feature of addiction.
Cravings are particularly common with certain drugs, including alcohol, nicotine, opiates and cocaine. Moreover, not only do cravings play this intrusive role in active drug use, but these unwanted desires can arise and be highly motivating even years into recovery from addiction. Craving is a major predictor of relapse. A systematic review of studies assessing the link between craving and substance use by using a method that evaluates craving episodes in real time in daily life found that in 92 per cent of studies craving was linked to substance use and relapse. Cravings can repeatedly override plans and resolutions to moderate or abstain from drug use, and this can be a disruptive, frustrating, demoralising and traumatising experience for those who battle these cravings – an experience that for some lasts a lifetime.
A lot of medical and clinical thinking about addictive craving is driven by a certain neuroscientific picture that explains cravings in terms of the effects of drugs on the production of dopamine in the brain. On this picture, the object of a craving is a drug itself or the pleasurable effects that getting high is expected to produce. But, by focusing narrowly on the brain, this view misidentifies the object of craving in addiction, or at least puts too much emphasis on the chemical component. When we look at the social and psychological factors that correlate with addiction, the real object of craving is made salient. In truth, addictive cravings seek out vital emotional experiences. They aim at numbing out, feeling in control, or feeling socially connected. Experiences such as these become particularly valuable and simultaneously elusive under certain environmental conditions. Understanding the object of addictive craving in this way helps to explain why cravings in addiction are so hard to resist.
The craving brain
One of the most popular dopamine-based explanations of craving focuses on reward-learning. While some of our desires may be hardwired, most are learned and are very malleable. The mainstream view is that this learning depends on the dopaminergic system. Phasic dopamine is a reward prediction error signal: it signals to animals, such as us, the difference between the actual amount of reward in the world at a given moment and the amount of reward anticipated. Bursts of dopamine are released when unexpected rewards, or unexpected cues that signal rewards, are encountered. These bursts tell us to act when we come across rewarding objects or related cues in our environment.
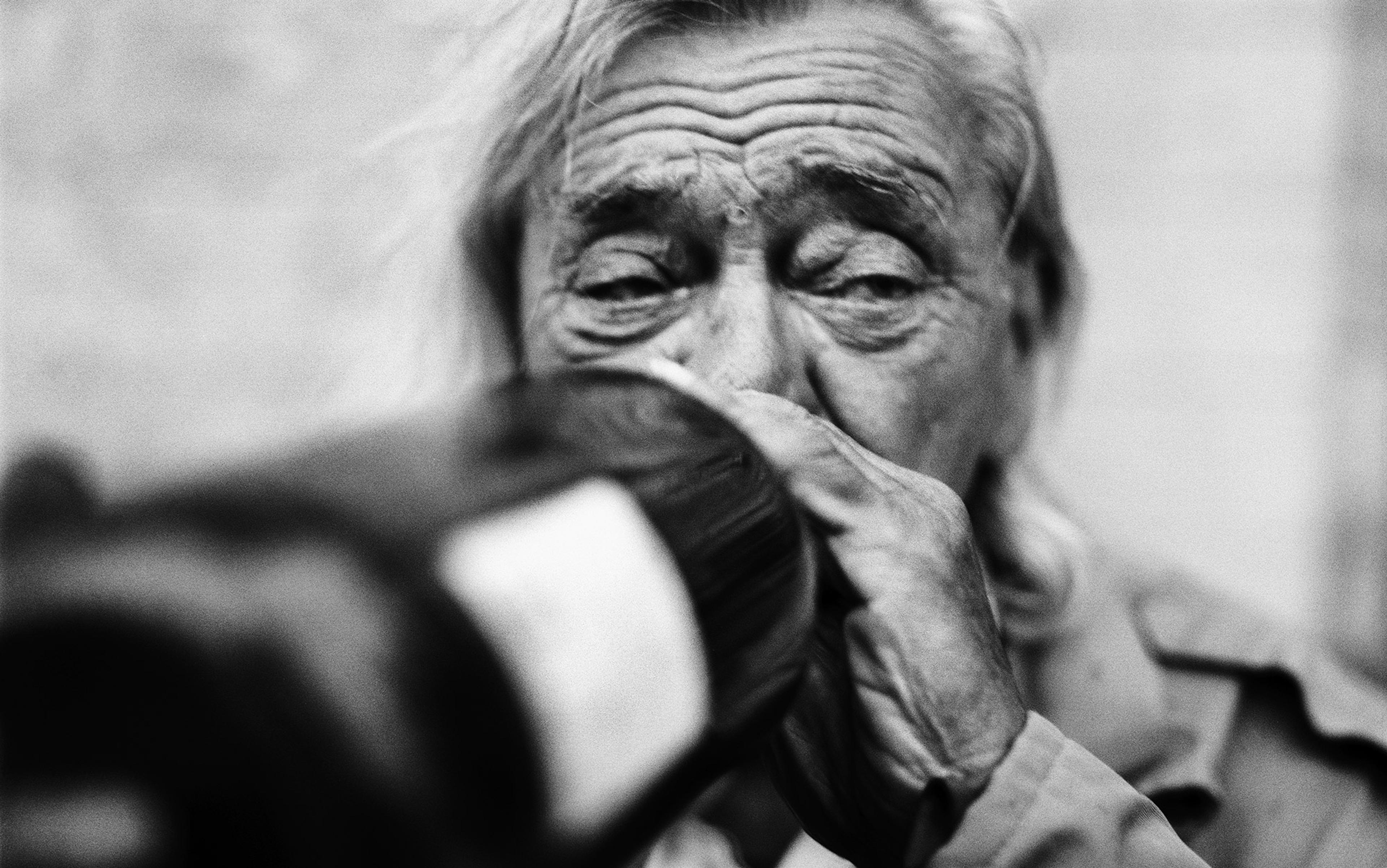
Cues can take the form of drug paraphernalia, but also locations, emotions and contexts
Addictive drugs have a pathological effect on this system. While there are various interpretations of the exact role of dopamine, it is well established that psychoactive drugs cause artificially high bursts of phasic dopamine to be released by midbrain dopamine neurons. Increased dopamine activity has been observed, for example, with the ingestion of amphetamines, alcohol, nicotine, opiates, cocaine, cannabis and benzodiazepines. When drugs are encountered, dopamine is released in anticipation of reward, but then the drug itself – due to its chemical effects – causes an additional dopamine boost when ingested, signalling that the drug is ever increasing in value. The result, on this mainstream view, is that these boosts in dopamine trigger cravings that overestimate the amount of reward that is expected, and so explain the excessive motivational pull of cravings.
Through repeated drug use, environmental cues become associated with drug-taking, and eventually these cues themselves start to trigger cravings. Cues are person specific and can take the form of drug paraphernalia such as needles or pipes, but also locations, emotions and contexts that have become associated with substance use. As a result of the long-term effects of this learning process, drug cues can continue to trigger cravings even years after active drug use has stopped, thus the link between craving and relapse.
The long-term effects of drugs on the brain’s reward systems are one reason why addiction is considered to be a chronic, relapsing disorder or neurobiological disease by the orthodox medical conception of addiction. On this view, addictive cravings are desires for the high produced by drug ingestion. These desires are abnormally strong, dysfunctionally caused, and they come to dominate the decision-making system.
Neuroscience tells only part of the story
While neuroscience offers insight into the brain mechanisms underlying substance use, explanations of craving have been heavily skewed towards studying the brain, with research funding being disproportionately allocated to biological causes. This promotes an incomplete and potentially misleading picture of addictive cravings. It is like studying humour by focusing on the brainstem nuclei that trigger laughter. Dopamine circuits operate in a larger context. To understand addiction, we must also look at experience, thought processes, behaviour, and life conditions. From this broader perspective, addictive cravings do not look like simple switches in the brain. Research shows that addiction is not automatic and, in most cases, not chronic.
First, it is not automatic. If excessively strong cravings were simply the result of drugs corrupting the reward systems in the brain, they should be produced across individuals who use drugs repeatedly over time. This is not the case. Most drug use does not lead to addiction, even the drugs that are often considered ‘highly addictive’, such as cocaine. One survey in the United States found that 19.4 per cent of people 12 and older reported past-month ‘illicit’ drug use, whereas only 3 per cent qualified for a past-year illicit drug use disorder. Drugs aren’t inherently dangerous, and not all drug use has negative consequences.
Why do cravings seem to weaken or desist over time for many addicted people?
Second, most cases of addiction aren’t chronic. Most people who do develop an addiction ‘age out’ of it without professional intervention. Over time, whether with the assistance of some form of treatment or not, most people decide to reduce or abstain from drug use, and they do so. For example, the majority of people who have an alcohol use disorder reduce or resolve problematic use over time. The case of Vietnam veterans and heroin addiction provides a concrete illustration of high remission: 20 per cent of US soldiers returning from Vietnam met the criteria for heroin addiction diagnosis while they were in active service, while only 1 per cent did before serving; of those who developed an addiction, 95 per cent were in remission within a year of returning home.
If addiction were simply the result of the brain being rewired through reward-learning, it shouldn’t be the case that so many people recover. Rates of recovery suggest that addictive cravings either stop or become easier to resist, given the correlation between drug craving and use as well as relapse. We need to look beyond biological factors to find a complete answer to the questions at hand: why don’t addictive cravings impact all people who use drugs equally, and why do cravings seem to weaken or desist over time for many addicted people? Neuroscience paints a partial picture. In fact, it misses out on what may be the most important and definitive parts of how cravings come to take such a controlling role in the lives of people struggling with addiction.
The social nature of craving
To understand the puzzle of addictive craving, we need to think about what cravings are for. A clue is that research shows the distinction between those who are most vulnerable and those who are least vulnerable to addiction strongly correlates with a range of social, economic and psychological factors. These factors are general predictors of addiction and typically have cumulative effects. These include structural factors such as poverty, unemployment, housing instability, incarceration, and lack of access to physical and mental healthcare services; and there are social factors as well, including adverse childhood experiences, mental health issues, stigma, prejudice, discrimination, and social exclusion. Many factors are both social and structural, such as colonial violence, transphobia and homophobia. These are factors we can alter, and collectively we have moral imperatives to do so.
So how do these factors contribute to understanding addictive craving? First, they play a role in determining which of a person’s psychological needs are being met. Addiction is often most severe and hardest to recover from where precarious and oppressive conditions are disproportionally present in one’s life, be this in the form of incarceration, houselessness, the unpredictable psychic distress of mental illness/madness, or social isolation. These conditions propel addiction by producing or exacerbating unpleasant to unbearable psychological states that drugs can be used to alter. Challenging emotions and stress are well-known craving triggers.
When we look beyond simple brain mechanisms, it becomes apparent that substance use has personal significance. Ostensibly, the object of craving is a drug or the expected pleasurable effects of intoxication, but the desires driving ongoing addiction run deeper. People who use drugs want to numb out, to feel alive, to feel accepted or socially connected, to be freed from mental or physical pain (including withdrawal symptoms), to not feel anxious, to feel included. These emotional experiences themselves can become the objects of the desires driving addiction, and drugs are a vehicle to satisfy them, at least temporarily. A craving for a cigarette can be a desire for control and order in a stressful environment. An alcohol craving can aim at feeling comforted and safe. A craving for ketamine can be a desire to feel relaxed and relieved from worries. In severe addiction, a craving might aim at a feeling of complete self-annihilation, to be freed, no matter the cost, from the painful conditions of daily life.
These are not simple urges to be high; they are psychologically complex, even existentially loaded states. Like much of human behaviour, these motivations are not always conscious and often only accessible on deeper analysis. When we think of the precarious life conditions that correlate with addiction, it’s unsurprising that yielding to these kinds of emotional experiences is significant. The desires to attain them through drug use, even in the face of consequences, reveal the social and structural conditions that characterise their absence.
Addictive cravings are reverberating echoes of the world within which one’s addiction develops
Social and structural factors can impose constraints on action selection, since they limit opportunities for addressing psychological needs. Drug use allows valuable control of psychological states when other means of addressing distressing conditions are hard to access or not accessible. Drugs are a non-ideal but available option for many people who experience disproportionate distress and are in various ways marginalised from social and institutional resources and supports. For example, one of the most significant correlates of addiction is other mental health diagnoses. A US national survey found that, in 2018, 49.4 per cent of adults 18 and older with a serious mental illness used ‘illicit’ drugs, compared with only 15.7 per cent of adults with no mental illness. Social factors (stigma and lack of supportive social relationships) and structural factors (discrimination and lack of access to mental healthcare services) constrain a person’s options for coping with the symptoms of mental illness, that is, for fulfilling the desires to alter these psychological states.
A particularly devastating feature of addiction is that, while drug use can become a way of addressing psychological needs, addiction can simultaneously increase life instability and exacerbate barriers to social inclusion and access to services, as people who use drugs face stigma, community exclusion and institutional discrimination.
From a social and structural perspective, addictive craving is not an involuntary switch but a strategy for coping with highly specific life experiences and conditions. Read an addiction memoir, speak to someone who has personal experience with addiction, or reflect on your own. Which drugs and particular experiences of intoxication become enticing, the initial reasons for trying them out, the roles they play in social interactions, all reflect cultural context, social norms and personal history.
Addictive cravings are responsive to the external environment. They are reverberating echoes of the world within which one’s addiction develops. The powerful motivation of craving is determined not only by how drugs affect the dopaminergic system, but also by the social and structural conditions that inform these desires in an individual’s life. These conditions are longstanding, and they shape the objects of craving in highly personal ways. What this teaches us is that a change in those external conditions can reduce cravings or make them easier to resist by deflating the significant emotional role that drugs are playing instrumentally.
What about genetics?
It might seem that an important piece of the puzzle has been neglected: genetics. This is often thought to be a major factor in addiction. For example, children of alcoholics are at four times higher risk of becoming alcoholics themselves. According to the US National Institute on Drug Abuse, approximately 40-60 per cent of the variation in the population in risk factors for addiction can be accounted for by genetics. Even so, this leaves around half of the variation to be explained by other causes.
Moreover, many people with a genetic predisposition to addiction never become addicted. Environmental factors play an important role in controlling the expression of genes, meaning that individuals’ genetic vulnerability to addiction depends on their circumstances. For instance, exposure to stress enhances this vulnerability, and having strong family and community connection protects against it. And anyway, genetics aren’t always at issue; many people without a family history of addiction do end up addicted nonetheless.
Addiction recovery isn’t just a personal health journey, it’s a collective struggle for social transformation
And what does this mean for craving? Even where heritability is at play, this leaves open how genetics influence the unequal distribution of addictive cravings. One possibility is that genetic variation in the dopaminergic system makes some people more susceptible to addictive cravings. But there are other possibilities, for example, that a genetic predisposition to stress sensitivity explains why some people in precarious life conditions turn to drug use to cope emotionally, while others do not. A social explanation of craving is not incompatible with evidence that genetics are a risk factor for addiction.
Three takeaways
How we think about addictive craving has impacts on how we think about addiction research, treatment and recovery, as well as how we think about the meaning of cravings beyond addiction. What follows from viewing addictive craving through a social and structural lens?
1. How we study addiction
The neurobiological explanation of craving on its own is unequipped to answer questions about why the desires driving addiction in key moments manifest unequally across individuals, and why they are so hard to resist. This doesn’t mean that addiction neuroscience is incapable of engaging with such questions. But more fruitful addiction neuroscience must do more than concede that social factors impact vulnerability to addiction. Social factors need to be integrated into research on addictive craving. Some neuroscience is already taking a more socially integrated approach to addiction, but this remains more of a rarity.
2. Rethinking treatment
Given the role cravings play in addiction and relapse, craving can be a crucial target for addiction treatment and intervention. If we view the strength of addictive cravings as primarily the result of how drugs affect an individual’s brain, then the most promising avenues for treatment would seem to be pharmacological interventions aimed at abstinence-based recovery, and therapies focused on individual strategies for coping with cravings. While we shouldn’t disparage any form of treatment or intervention that helps some addicted persons, we need to be realistic about the limited impact of addiction neuroscience research on advancing clinical treatment, and about the limits of therapies focused on individual self-control when one’s environment remains unchanged.
A more socially integrated explanation of craving affirms that treating addictive craving requires addressing the socioeconomic, structural and emotional conditions of individuals experiencing addiction. Identifying and addressing adverse social conditions should be a key element in the fight, and this too often goes ignored. We need to do this in treating patients, and at a broader, societal level. Focusing narrowly on the brain to explain craving also misses the ways that the modern world is perfectly built for the desires driving addiction: capitalism, poverty, inaccessible healthcare, colonialism, the prison industrial complex, child abuse, an increasingly socially disconnected way of life. A social view of craving promotes the perspective that addiction recovery isn’t just a personal health journey, it’s a collective struggle for social transformation.
3. The wisdom of cravings
Philosophically, the takeaway is that cravings are not simple, visceral urges or control forces aimed at drugs or the immediate effects of intoxication – cravings are richer, more cultural, cognitive, and phenomenologically complex than that. This has implications for cravings beyond addiction. Cravings are sensitive to emotional and psychological needs and values, and this helps to explain why they are so motivating. Imagine a mundane craving to check Instagram or Twitter. Built into that craving, one might also find a desire for attention, validation, social connection or interaction, a cure for loneliness, emotional numbing, maybe the self-punishing urge to compare and despair, or for what the philosopher Jean-Jacques Rousseau called amour-propre, a form of self-love that is constituted by the recognition or approval of others. Next time you find yourself having a craving, reflect on how you experience it. Is it your brain anticipating a spike in dopamine, a flood of pleasure? This may be part of the story. But does it also mean something more to you? Is it serving some greater purpose?