The ancient Greek physician Hippocrates defined health as a body in balance. The human body was a system of four coordinated humours (blood, black bile, yellow bile, phlegm), each of which had its own balance of qualities (hot or cold, wet or dry) connected to the four elements (fire, air, earth, water). The balance of these qualities and humours was inextricably linked to environmental conditions. Phlegm, for instance, was connected to the element of water, and had the qualities of cold and wet. Hippocrates recognised that when this bodily system was exposed to conditions that perturbed or exacerbated its humours, such as the cold and wet of a snowstorm, the system became unbalanced, in this case producing too much phlegm. His treatments for an abundance of phlegm focused on removing the excess humour and increasing the yellow bile (hot and dry) to bring the body back into balance. Today, we might identify such a condition as a respiratory disease. Hippocrates would not have identified the condition so locally. He would have considered it a condition of the whole body: ‘dis-ease’ was literally a system out of ease or balance.
Today we think less about the whole body as a complex system and more about its parts and sub-systems. An X-ray of the lungs shows congestion, so we assume the problem is in the lungs and treat for pneumonia, not worrying about other parts of the body unless they show their own symptoms. If a culture in the pathology lab shows a particular microbe at work, we prescribe the relevant antibiotics to combat that microbe rather than attempt to rebalance the system as a whole (despite the current trend to add ‘probiotics’ to the antibiotics approach). This move toward localised diagnoses began in the 18th century with the rise of morbid anatomy and the localisation of symptoms to parts. The French physician René Laënnec’s invention of the stethoscope in 1816 allowed him to hear various abnormal sounds in the chest of a patient suffering respiratory distress. He could then carry out an autopsy after the patient died and correlate the visibly abnormal parts with the symptoms that he had detected, which led to powerful diagnostic tools.
The result was the localisation of abnormalities to particular parts of the body, which led to the concept of localised diseases and the need for specialised treatments. Modern medicine celebrates the ability to diagnose problems based on localisation of symptoms. The systemic imbalance or ‘dis-ease’ of Hippocrates thus became a growing set of separate diseases associated with specific causes, dissociated from the notion of the body as a system.
Following the localisation of diseases came the specialisation of treatments. These treatments typically rely on identifying the problem within a particular part or subsystem and fixing it, with the goal of getting the patient back to ‘normal’. If a physical part is damaged, we want to repair it so that it works again as closely as possible to the way it was working before. Or, if it cannot be fixed, perhaps because a limb was cut off or a kidney failed, then the tradition has been to replace it with something as close as possible that will work the same way: prosthetics for lost limbs, dialysis machines for failing kidneys.
Despite vast differences in understandings of disease and treatments, models of health from Hippocrates to modern medicine have focused on reestablishing the same state as occurred before illness. Health is a concept imbued with a sense of stability; it is constituted by a body returning to a state that existed before disease or injury and the maintenance of this state. Stability is therefore understood as the maintenance or regeneration of a single, ‘healthy’ state of the body. Since this approach has saved vast numbers of lives, medicine applauds the invention of new analytical tools, procedures and treatments that advance an understanding of health as a return to a previous state. The sense of stability implicit in thinking about health leads to a picture of health as an outcome of regeneration: a body damaged by injury or disease is brought back to, or regenerates, a previous, ‘healthy’ state.
But what if health isn’t simply a return to a previous state? If we think about health as part of a larger framework of considering organisms as complex systems, there is no ‘return’. Complex systems shift in response to environmental challenges; they adapt to their conditions in order to survive – and adaptation breeds change. Framing health in terms of regeneration, and then asking what it means to regenerate, allows us to prod our assumptions about health as a singular, predetermined outcome and rethink our values in sustaining complex systems in light of damage. That raises the question: what does regeneration mean?
In 2017, we formed the McDonnell Initiative at the Marine Biological Laboratory in Woods Hole, Massachusetts, which brought together historians, philosophers and scientists to investigate what regeneration means across multiple scales of life. Regeneration is typically thought of as renewal, revitalisation, rejuvenation, repair, recovery and a lot of other re- words. The ‘re-ness’ suggests return to prior conditions. Together, the authors of this essay explored the concept in the history of biology, asking what regeneration has meant when applied to individual organisms, especially through the 20th century. Others in the McDonnell Initiative have been looking at what regeneration means for microbial communities, germline, nervous systems and ecosystems.
In our book, What Is Regeneration? (2022), we laid out ideas of regeneration arising in the 18th century and looked closely at the contributions of early 20th-century biologists. Led by René-Antoine Ferchault de Réaumur and Abraham Trembley, 18th-century naturalists made meticulous and detailed observations of organisms responding to injury. In the first decades of the 18th century, Réaumur watched as crayfish limbs slowly regenerated, documenting different stages of regrowth that led to a complete replacement of the lost limb. A few decades later, Trembley cut hydra into various pieces, and discovered that they regrew all of their lost parts. Writing in 1989, Howard and Sylvia Lenhoff convincingly argued that Trembley saw the organisms he worked with as living systems – he looked at the interacting whole, its structure, function and behaviour. Réaumur and Trembley, and others at the time, saw regeneration as a process of repair and replacement, bringing organisms back to their previous states, akin to the notion of stability we see in medicine.
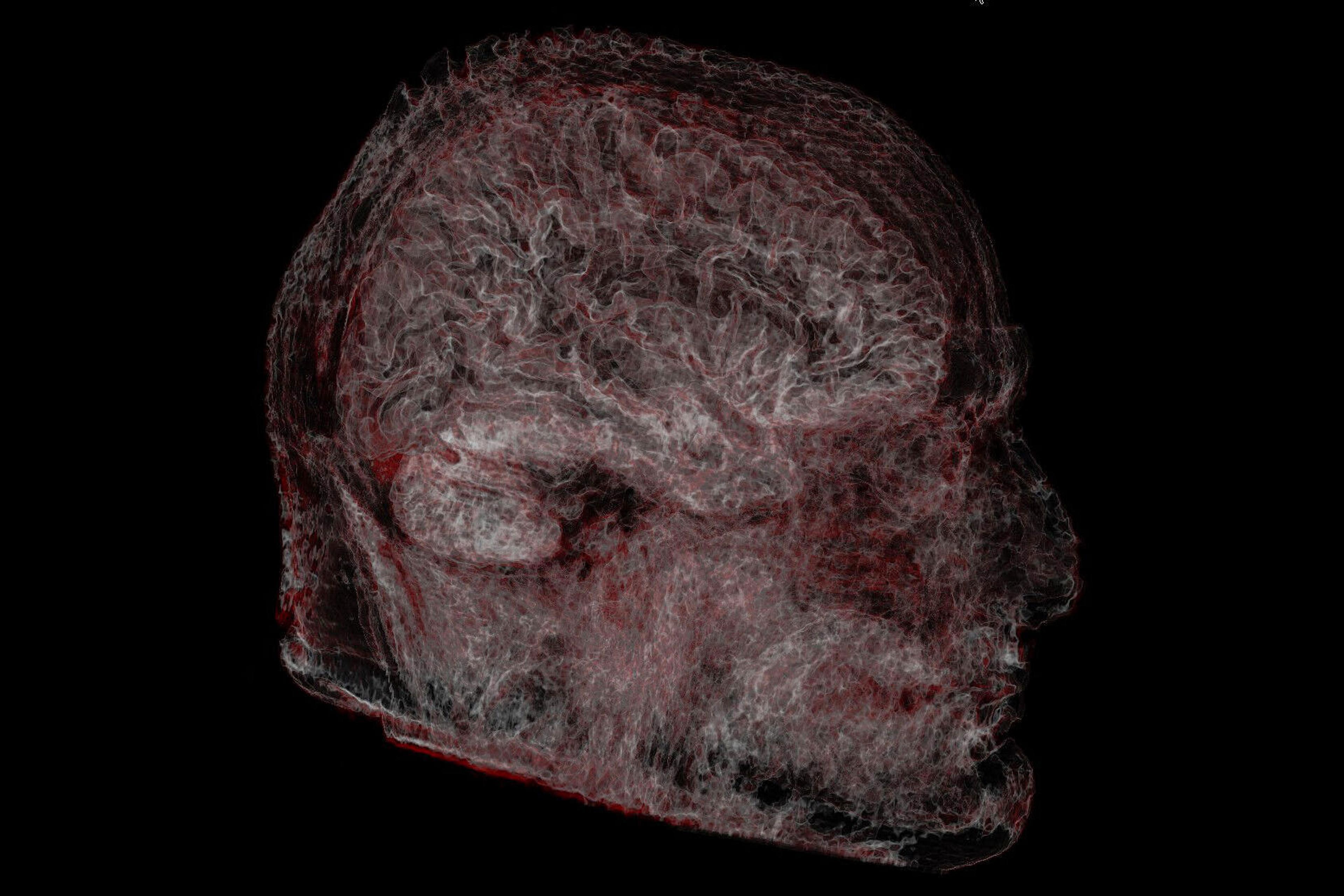
In 1901, the American biologist Thomas Hunt Morgan summarised what was known about regenerating organisms, from both his own studies and preceding explorations. Morgan experimented on a broad swath of organisms, building up evidence for his argument that scientific claims should be grounded in experimentation and devoid of theoretical speculation. Perhaps his most stunning insights came from planarian worms. After he cut them into various bits, he found that they could regenerate, producing a new tail, middle or even a fresh head, if needed. Some experiments even showed planarians regenerating a second head on the posterior of the old head after the body had been removed, a marked departure from the planarian’s previous state.
A stable system might in some senses be even more healthy than what was there before
What about hydra? Morgan turned them inside out, cut-and-pasted various parts together, and they kept growing and remained alive. These were most definitely not in the same condition as they were before his experiments – their bodies, through the regenerative process, had transformed into new and curious systems. Or, as Morgan put it, ‘a change in one part takes place in relation to all other parts, and it is this interconnection of the parts that is one of the chief peculiarities of the organism.’ Morgan joined other researchers at the Marine Biological Laboratory in marvelling at the variety of responses these organisms could make when responding to changing contexts and conditions.

Regeneration of planaria, from Regeneration (1901) by Thomas Hunt Morgan. Courtesy the Wellcome Collection, London

Regeneration of hydra, from Regeneration (1901) by Thomas Hunt Morgan. Courtesy the Wellcome Collection, London
One of those biologists was Jacques Loeb, who saw the potential to go further than just experimenting and describing what the organisms did. He imagined being able to engineer the results, to use the scientific knowledge about what organisms do during regeneration in order to control the results of this process and improve on what happened normally. The result would be a stable system that might in some senses be even more healthy than what was there before.
The works of Morgan and Loeb offer definitive shifts from previous views of regeneration, and they show us two important things. First, they brought to fruition Trembley’s early views that regeneration is a process that occurs within a living system. A system is a group of parts that interact in a coordinated fashion. The resulting whole follows rules and principles, which allow some kind of communication and integration of the parts so that the entire system is responsive and regulated as well as stable. Stability, then, meant not a return to a previous state, but the ability of a system to maintain its coordination and communication among parts. Morgan and Loeb understood that an intervention on one part would, in some way, affect the entire organism, much in the same way that Hippocrates understood that disease affected the entire body.
Second, Morgan and Loeb show us that regeneration does not simply mean a return to ‘normal’ like the 18th-century naturalists believed. Rather, they saw regeneration as an adaptive process. These men were not evolutionary biologists and did not think of adaptation in evolutionary terms of species adapting to a changing environment over geological periods of time. Instead, they emphasised adaptive responses of individual systems to stimuli affecting the individuals, a more proximal sense of adaptation. They did not think in terms of replacing particular localised cells or tissues or organs, but rather in terms of stimulating the organism to respond by repairing damage for the whole. They saw the individual organism as a complex system, and one that adapts to its changing environment by initiating repair.
Skipping forward toward the 21st century, we find many life scientists embracing this notion of regeneration as a process in adaptive systems. Research on gastrointestinal microbial communities has shown that when the community is perturbed by antibiotics, it will reform, but the microbes will be different, and so will their community interactions. Experiments on lampreys indicate that, when spinal synapses regenerate following injury, the regenerated synapse is morphologically distinct from its pre-regenerative state, even if it performs much the same function.
All of this research indicates that regeneration is, broadly conceived, the adaptive process by which a living system responds to a stimulus and maintains its stability. Adaptive, in this context, means that systems change through the process of regeneration in response to both internal and external conditions. Stability means that the system remains able to coordinate its parts. A system before regeneration will never be identical to a system after regeneration; there will always be changes in the parts or the relationships between them, even if they look or function the ‘same’.
What appears to shape the results of regeneration is context. Whether that context is the microenvironment of a cell, a tissue, the entire body, the body within its environment or all of these, context is an essential part of regeneration within the complex system because it provides the fodder for the adaptive response. As the biologist Michael Levin and the philosopher Daniel Dennett pointed out in their Aeon essay: ‘The great progress has been mainly on drilling down to the molecular level, but the higher levels are actually not well-off … We know how to specify individual cell fates from stem cells, but we’re still far from being able to make complex organs on demand.’ Despite decades of enthusiasm for molecular biology and genetics, we can’t rely on knowledge of the molecular alone – we also need to be able to understand how molecules, cells, tissues and the body within an environment interact in order to move towards repair of individual organisms. And it is not just the higher levels of the individuals’ structure and function that shape adaptive responses to environmental changes, but also the context in which they exist.
Because living systems regenerate by changing and adapting to both internal and external stimuli, understanding health as simply about stability in the sense of being fixed, as recovering a system to its condition before a stimulus, doesn’t quite make sense. The concept of regeneration embodies Heraclitus’ famous saying: ‘You cannot step in the same river twice.’ If we consider health as an outcome of regeneration, and regeneration is an adaptive process, we should lean into regeneration and adaptation when considering health. Research at the intersection of complex systems and health outcomes has shown that poor health states are closely linked with loss of adaptive responses within complex systems. We want to focus on the bigger conceptual picture and not get swept away in the details of thinking about the dynamics of complex systems. Extrapolating from lessons in regeneration biology to conceptions of health has many consequences, but we want to explore two, intertwined changes: how this adaptive view of regeneration alters our thinking about goals and outcomes of health, and what this means for our values related to health.
If we’re not tied to the position that systems must return to a previous state, then we can explore alternatives. After all, if we don’t take the previous state of the system to act as our target outcome, we have to select what we want the outcome – or the range of possible acceptable outcomes – to be. If we want to intervene in a system, for instance chopping off the salamander’s limb, severing the lamprey’s synapses or manipulating planarian genes, our expectation cannot be fidelity to a pre-diseased or pre-injured state. Instead of focusing on replacement and repair towards reestablishing the state before illness, we can focus on what would be the ideal state for that goal. Is it necessary that the salamander regenerate a limb of the same size, or might it work just as well to have a smaller limb that takes less energy to regrow? Perhaps the new synapses that bypass the damaged site in the lamprey can be more efficient because they ‘know’ what path to follow? Or knocking out genes in planarians may allow other regulatory pathways to work and reveal connections among the genes, cells and resulting organism.
The question of ‘what constitutes an ideal state’ is one of values
Now let’s consider this focus on choosing outcomes within human health. Despite more than 3,000 years of fashioning prostheses to replace missing parts, today around 20 per cent of people outfitted with a limb prosthesis end up abandoning their device, often because it doesn’t feel or work ‘right’. There has been a great deal of research in improving functionality of prosthetic devices, less in improving comfort, and far less in understanding psychosocial factors that contribute to device abandonment. From our new perspective of health as an outcome of adaptive regeneration, we can begin to ask questions about the goals we want to achieve: do prosthetic devices need to mimic the form of the lost structure? If functionality is the primary concern of most prosthesis wearers, are there other ways to achieve functionality? And are prostheses always the best solution? While this is not the place to address the vast and richly informative literature on ableism and embracing different abilities, it is worth noting that thinking about regeneration as promoting a range of different approaches to the health of a complex adaptive system offers parallel challenges to the assumption that all organisms need to be the same to be considered whole and healthy.
This brings us to the second shift in perspective about health: values. The question of ‘what constitutes an ideal state’ is one of values. After all, if health is possible within an array of outcomes, we have to select what we want the outcome to be. Whatever we select will be based on what we deem most important – that is, what we value. Hippocrates realised this when he emphasised health as a balance of elements within the whole system. If asked ‘rebalance for what?’ he would have said ‘health’. We can ask an updated version of his question concerning regeneration: regeneration for what? When intervening in a system to promote health, should we privilege enhanced function? If so, which functions do we want to optimise?
Picturing health (and regeneration) through this lens of rebalancing the health of the whole has a bearing on the transhumanism movement, which asks similar questions. In both cases, we also need to recognise who is asking and answering the question: the patient? The clinician? The biomedical researcher? Each of these stakeholders may have a different sense of what health is. Being clear about our goals is a starting point, and reflecting on the terms we use is another major step toward opening our minds to different – and perhaps better – ways to think about health, the health of organisms including humans. We do not have the answers, but we have offered suggestions to think in terms of complex systems that are adaptive to change and therefore themselves change over time. Plus, we invite robust discussion about what our goals of health should be if we embrace the idea that it is not always best simply to go back to what we had before. Health is more complicated than that.