‘Some, pale and depressed by inanition, swooned away and died, stretched on the snow … They were seen walking insensible and ignorant where they went … In a word, when no longer able to continue walking, having neither power nor will, they fell on their knees … Their pulse was small and imperceptible; respiration, infrequent and scarcely perceptible in some, was attended in others by complaints and groans. Sometimes the eye was open, fixed, dull, wild, and the brain was seized by quiet delirium.’
It was the French doctor Pierre Jean Moricheau-Beaupré who provided this recounting in A Treatise on the Effects and Properties of Cold (1826), one of the most complete, original descriptions of hypothermia, the condition in which body temperature falls dangerously low, below 95°F or 35°C. He was writing of his experience on the Napoleonic retreat from Moscow in 1812, almost 80 years before the medical term was coined.
Hypothermia has its Greek origins in ‘under’ (hypo), and ‘heat’ (therme). Its symptoms depend on the extent of temperature decline but initially involve shivering, poorly coordinated, laborious movement, and disorientation. At extremes, heart rate decreases significantly while retrograde amnesia and confusion set in. After further decline, victims can begin to make irrational decisions and talk incoherently. For reasons poorly understood, they’ve even been known to take off their clothes and seek confined spaces before death reigns.
Yet today, this insufferable condition is induced by physicians to slow down the metabolism so that patients can survive. After decades of contentious science, hypothermia now helps to halt the onslaught of adverse effects that cause death. Its therapeutic value lies in its ability to suspend the physiological needs of cells; after all, if cold cells in torpor don’t require much oxygen and other nutrients during or after trauma or cardiac arrest, when blood flow has stopped, it will take that much longer for those cells – and the patient – to deteriorate and die. The connection between hypothermia and out-and-out ‘suspended animation’, the frozen state that many hope will preserve us through years in space on our way to Mars and Earth 2, is no coincidence. Although the exact mechanisms are complex, hypothermia slows down metabolism, delaying the destructive effects of oxygen loss until normal blood circulation returns.
The new field of therapeutic hypothermia has even begun to reframe the boundaries of life. In the past, the Rubicon between life and death was the absence of a heartbeat. Later we learned that the brain could survive the lack of a pulse for a while, and people suffering from heart death were brought back from the brink as long as their brains stayed intact. But without circulation, a brain could last only so long.
In recent years, however, advanced methods of hypothermic cooling have slowed brain activity to a crawl, pushing the borders of death way beyond the moment when the heart stops. Among other benefits, these advancements have allowed researchers to expand their studies of the near-death experience with reports from those who have been heart-dead for ever-longer periods, but then come back. They have also reignited research into human hibernation with the aim of hypothermic cooling for astronauts venturing into interstellar space.
Cold therapy was first used as a localised treatment. Some of the earliest documented applications include those found in the Edwin Smith Papyrus – the most ancient medical text known, dated to 3500 BCE – so named after its owner, who bought it from a dealer in Luxor in 1862. It describes the Egyptians’ use of cold for treatment of abscesses. Later, around the 4th and 5th centuries BCE, the Hippocratic School of Medicine in Greece suggested packing patients in snow to treat haemorrhage, likely by constricting blood vessels. But it wasn’t until the late 18th century that James Currie, a physician in Liverpool, conducted the earliest-known whole-body hypothermic treatments. He immersed healthy volunteers, who must have been dedicated, in water as low as 6.5°C for up to 45 minutes in an effort to find a way to treat mariners suffering from cold-water trauma after a shipwreck. His pursuits were facilitated by significant improvements in the accuracy of thermometers.
After the dawn of modern medicine, when it became standard for trained doctors to diagnose and treat ailments by means discovered through science, things changed. The controversial, pioneering research of the American neurosurgeon Temple Fay provided fuel. While still a medical student in the late 1920s, the story goes, Fay was asked why metastatic cancer rarely appeared in the limbs. He didn’t have the answer at the time, but ultimately noted that one’s limbs exhibited relatively low temperatures. He ingeniously connected this fact to a discovery he made on his farm in Maryland – that lowering temperature inhibited the growth of embryonic chickens. From there he hypothesised that cold could be used to treat and prevent cancerous growth. It was a ‘Eureka!’ moment. By 1929, he had achieved a professorship in neurosurgery at Temple University in Philadelphia. Soon he began using basic methods of whole-body cooling, packing patients in ice, for example, and devising various implements for localised cooling – this included sizeable devices, crude by today’s standards, to be inserted within the skull.
She survived in freezing water under a layer of ice, and went for hours without a pulse before regaining a heartbeat
But his raw methods provoked criticism and anarchy in the hospital ward. He used giant tubs of ice – up to 150 pounds worth – in the operating room for periods of up to 48 hours. The melt would cause constant flooding that had to be soaked up. Moreover, rooms were cooled simply by keeping the windows open, exposing not only the patients, but the entire medical staff to the often frigid local winters. On top of that, back then it was daunting to accurately measure a patient’s body temperature without proper (usually rectal) thermometers designed for the purpose. (Thermometers back then weren’t calibrated to read temperatures below 34°C.) This made Fay extremely unpopular among the nursing staff, who, according to one report, declared mutiny against his human ‘refrigeration service’.
Yet, Fay was brilliant. In one of his early reports, he cited a mortality rate of 11.2 per cent and a 95.7 per cent rate of success in pain relief as a result of his refrigeration therapy. Crucially, these experiments revealed not only that humans can endure a hypothermic state for days, cooled as low as 32°C, but also that they can be revived with significant improvements to their condition.
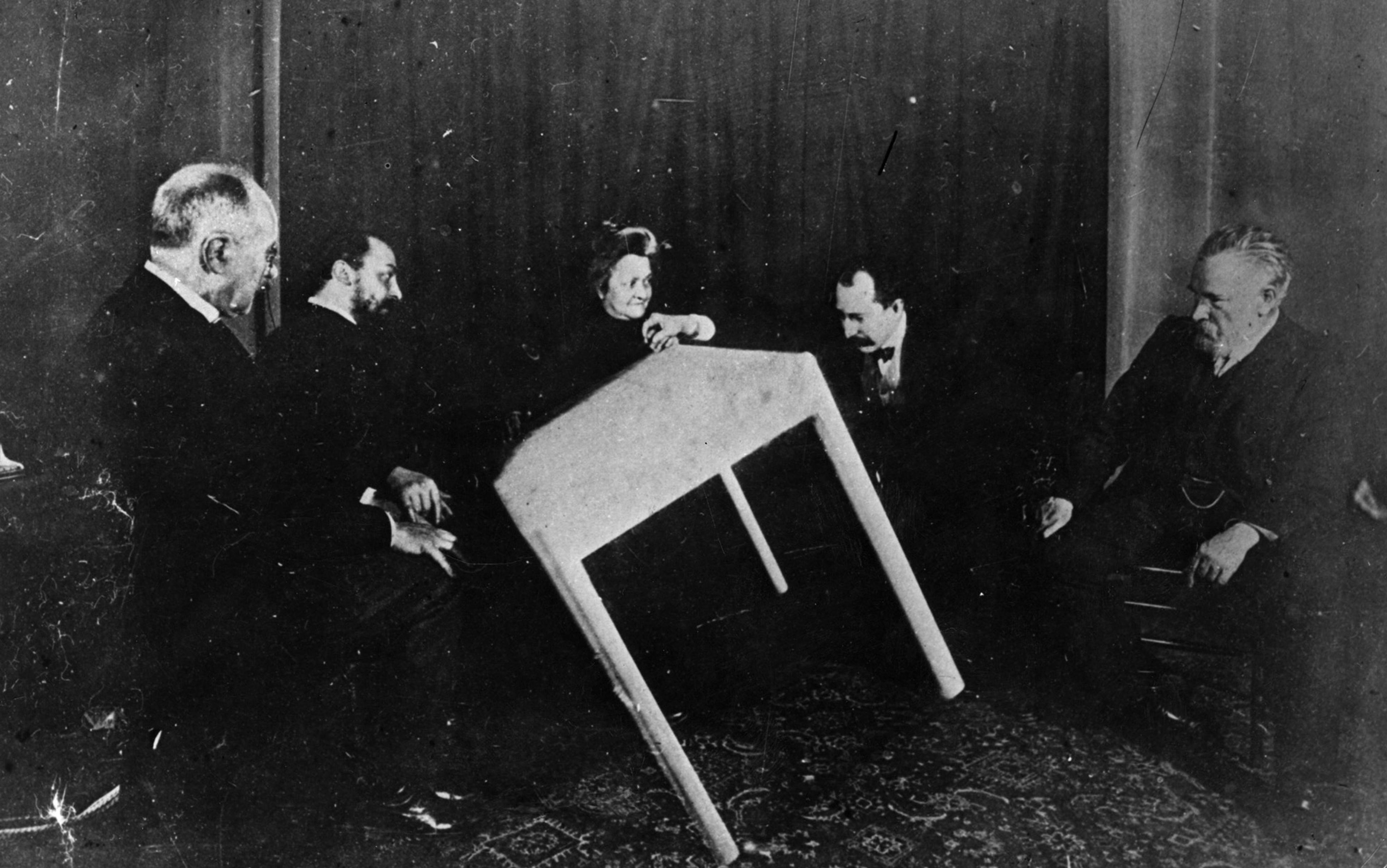
Tragically, in a sudden and criminal turn of events, these early reports were seized by the Nazis and used in hundreds of brutal experiments during the Second World War. Prisoners were forced into tanks of ice water with a ‘wait and see what happens’ approach to experimentation. The data has since been declared unscientific. The association with torture stagnated further research for decades. After all, this was still at a time when the term ‘thermal barrier’ implied that a body temperature below normal was to be avoided at all costs.
It wasn’t until the mid-1980s that the pioneering anaesthesiologist Peter Safar, born in 1924 in Vienna, daringly practised therapeutic hypothermia research, despite its stigma. Working at the University of Pittsburgh with dogs as a medical model, he confirmed that, after a cardiac arrest, a mild hypothermic brain temperature (33-36°C) significantly improved neurological outcome and prevented brain damage. Safar successfully reinvigorated hypothermia research with these findings. The treatment he invented was called ‘suspended animation for delayed resuscitation’.
The science of therapeutic hypothermia was further motivated by the extraordinary cases of patients who survived cold-water drowning – take, for example, the trainee doctor Anna Bågenholm, who suffered a cardiac arrest after a skiing accident in northern Norway in 1999. She survived in freezing water under a layer of ice for 80 minutes, and went for hours without a pulse before regaining a heartbeat.
After the dawn of the new millennium, Joseph Varon, today chief of critical care at University General Hospital Systems in Houston, catapulted therapeutic hypothermia to new heights. It was 2005 when a vacationer was flown from Mexico to Houston after a drowning incident, Varon told me. ‘I flew him here to Houston. The guy was dead for a couple hours. They brought back his heart, and eventually we were able to cool him and not only bring his brain back, but he did very well.’ The case was subsequently reported in the journal Resuscitation. ‘When Pope John Paul II had a cardiac arrest that same year,’ Varon added, ‘I was asked to go to the Vatican – to cool him off.’
Varon, known to insiders as ‘Dr Freeze’, was, like Fay, initially viewed with skepticism by hospital staff. ‘When I started doing this in Houston, I used a lot of ice. I dropped the room to a very low temperature,’ he said. Before long, he was using hypothermia to protect his patients against neurological damage after a variety of traumas, including cardiac arrest, stroke and liver failure. His patients are routinely cooled to temperatures as low as 32°C – for as long as 11 days. And in 2014, he used hypothermic treatment to save his own life after suffering a stroke. ‘The first thing that came to mind was: Cool me off!’ Varon told me.
And eventually his technique improved. Today, Varon uses a variety of advanced devices for administering both localised and whole-body hypothermia, typically to chill patients to 32°C during recovery from cardiac arrest, after their hearts have come back online. The technology includes machines that have hydrogel pads that circulate cold water to cool patients, a biofeedback mechanism for controlling temperature, and a computerised catheter that goes inside the leg, allowing the patient to remain chilled but awake – key for proper neurological assessment.
Moreover, in some cases of severe trauma from, say, a gunshot or stab wound, an extraordinary clinical trial is underway. Here, patients undergo profound hypothermia. They are cooled to 10°C, often while they have no heartbeat or respiration. Yes, this involves cooling the ‘dead’ – but could save their lives.
SpaceWorks’ current plan includes a short-term form of torpor, in which space travellers go into and out of the suspended state every two weeks
Cooling can prolong an otherwise extremely short window of time during which trauma victims can undergo necessary surgical operations, especially those required to prevent blood loss. A notable trial dubbed Emergency Preservation and Resuscitation (EPR) is taking place in Pittsburgh and Baltimore in communities that experience some of the highest trauma rates due to gunshot and stab wounds. EPR is used as a last resort, when standard methods of resuscitation fail, leaving the victim with a mere 5 per cent chance of survival. The procedure involves replacing a patient’s blood with a circulating, cooling saline solution, which prevents cell and tissue damage from lack of oxygen. When it is used, patients can regain a heartbeat after having no pulse for a duration of an hour. The aim is to compare 10 patients who received EPR with 10 who did not, to see if there’s an improvement in outcome, which here is life rather than death. Official results are currently kept under wraps, unavailable to the public.
But Samuel Tisherman, who heads the trial, is very upbeat. Long accustomed to pushing the envelope, Tisherman worked with Safar on ‘suspended animation’ during the 1980s, when he was in medical school. Now his study subjects are routinely cooled from a normal temperature of 37°C down to a staggeringly low 10°C over the course of about 20 minutes. Tisherman explained: ‘We need to do it fast because the person’s already lost pulse; the whole idea of this is to decrease the body’s need for oxygen.’ Particularly, they need to cool the heart and brain because those are the organs most susceptible to a lack of oxygen. Once cold, the patient, lacking pulse or any blood pressure, is moved to the operating room. Finally, under these extreme conditions, a trauma surgeon will attempt to fix the sources of blood loss and repair any other injuries. When this is accomplished, they start to warm the patient slowly. ‘The hope is that, once they are warm, the heart starts beating,’ Tisherman said.
When asked about the current progress of the trial after facing these issues, Tisherman paused and then with a gentle laugh said: ‘We’re doing it. That’s progress!’ We’ll have to wait for formal results, but a critical milestone seems near.
Beyond medical applications for the deathly ill, hypothermic cooling might one day be used for what most of us have come to know, through science fiction, as a type of suspended animation, in other words, human hibernation. The idea gained traction in the 1960s, during the space race between the United States and the USSR, and has recently been revived through what is now called torpor. Torpor offers a number of benefits for prolonged space travel. It can prevent medical complications, including muscle atrophy and bone-density loss, known to result from extended periods in a zero G environment. Beyond such preventative aims, it could also achieve some key psychological benefits. Loss of consciousness avoids both the extreme stress and extreme boredom that can come with months of space travel in a confined space, not to mention the interpersonal conflicts that would be likely to arise among a small crew over such an extended period.
Enterprises such as SpaceWorks, based in Atlanta, have received renewed funding from agencies such as NASA’s Innovative Advanced Concepts programme for human hibernation research. SpaceWorks’ innovative approach emphasises enormous savings on food, waste-disposal, storage and space requirements that would otherwise contribute significantly to the mass of the vessel and therefore the cost of the mission. ‘We approached them with a realistic idea and showed them the monetary benefit and the math to do it,’ said Douglas Talk, departmental director of surgical services at the Naval Air Station in Lemoore in California. He’s been working on the project for SpaceWorks since 2013. He told me: ‘I’m a doctor and a huge sci-fi nerd, and this is the perfect melding of those worlds!’
SpaceWorks’ current plan includes a short-term form of torpor, in which space travellers go into and out of the suspended state every two weeks, reducing metabolism by about 7 per cent per degree Celsius. ‘We know there are many mammals that hibernate so it’s not: Can mammals hibernate?’ Talk said. ‘It’s: How, and can we do it in humans? We know we can do it in the short term, and we even have studies that show it’s possible for two weeks.’ Talk is referring to a case in China in 2008, where a woman in a coma after an aneurysm was cooled for 14 days to prevent further brain damage and facilitate healing. Amazingly, she achieved a full recovery.
There’s a straight conceptual path from our current knowledge of hypothermic stasis to a Mars mission. Talk said the journey would start on a Moon station, where ‘astronauts would go to get some experience with torpor to know what to expect in terms of going into it and coming out of it’. SpaceWorks’ plan is to maintain the astronauts through a surgically-implanted IV line called a ‘mediport’, similar to those currently used for cancer patients undergoing chemotherapy. Sojourners would also have an oesophageal tube going into the stomach for feeding. ‘These things have very low complication rates. Once the crew has all their checks, they would go to the stasis module, and go into their beds, and hook their monitoring and food systems. And then we’ll lower the temperature of the habitat. How we’d initiate torpor is not how hospitals do it – they use a lot of sedating drugs. We would use pharmaceutical agents that drop core temperature down to 32°C and decreases metabolic rate.’
Creating such agents is a primary goal for Talk and his colleagues. Already, they have had success in pigs, which, he explained, is key because ‘it’s the first time anything close to hibernation has been achieved pharmaceutically in a non-hibernating mammal’. After training on the Moon, crew members would rotate in and out of stasis so that someone was always there to oversee the safety of the hibernating others.
Altering the nature of sleep across space and time could cause our human nature to change. The capability for ‘hibernation on demand’ could mean that we’ve transcended our intrinsic circadian ties to cosmic elements such as night and day. Our very genetic basis dictates a biology synchronised with the rhythm of the Earth’s rotation. Such tuning is necessary to regulate sleep patterns, eating times, the release of hormones, blood pressure and body temperature. These rhythms are an essential part of our humanity. If a state of hypothermic hibernation slows metabolic processes to a crawl, and suspends our rhythmic biological requirements, could it, for example, delay the effects of ageing? Might Martian travellers regain the time spent in hibernation on the long voyages to Mars and back? Or, thinking into the distant future, could interstellar explorers return to Earth centuries or even millennia after they left?
Talk was unsure if human hibernation would upend circadian requirements, but said it might be possible to find a fundamental, genetically-based hibernation trigger in humans. ‘State-of-the-art research suggests that there’s something called a HIT – a hibernation-inducing trigger,’ he said. ‘It’s some chemical that primes the body and triggers hibernation and the ability to tolerate the state of hibernation. I think that somewhere in our DNA is the ability to trigger hibernation in the same way, and that this ability has been lost in our evolution.’
Another challenge to our sense of self might come from expanding the boundaries of death. Once we defined death as ‘heart death’. When the heart stopped, we were gone. Then we broadened to ‘brain death’ – no brain waves meant you could never return. Now, hypothermic patients who show both heart death and brain death are being reanimated through hyperthermia, pushing the boundaries of life once again.
Consider the hospital in Norway where Bågenholm was treated after her ski accident in 1999. Prior to her admission, all incoming pulseless hypothermic patients died – a survival rate of 0. Yet once the hospital realised that patients could exhibit brain activity for hours, possibly even days after their heart stopped, they employed more aggressive attempts at resuscitation, increasing survival to at least 38 per cent.
Extreme cases of patients who come in frozen have altered our approach to death. In 2011, a 55-year-old man in cardiac arrest was brought to the hospital at Emory in Atlanta, and put into a hypothermic state for neuroprotection. After a neurologic exam, doctors declared him ‘brain dead’, and 24 hours later he arrived in the operating room for organ procurement. Yet, according to the subsequent report in the journal Critical Care Medicine, doctors then observed his corneal and cough reflexes and spontaneous respirations. Although there was no hope of reanimation (and he was not harvested alive), such cases throw into doubt the longstanding neurologic tests still used to determine time of death.
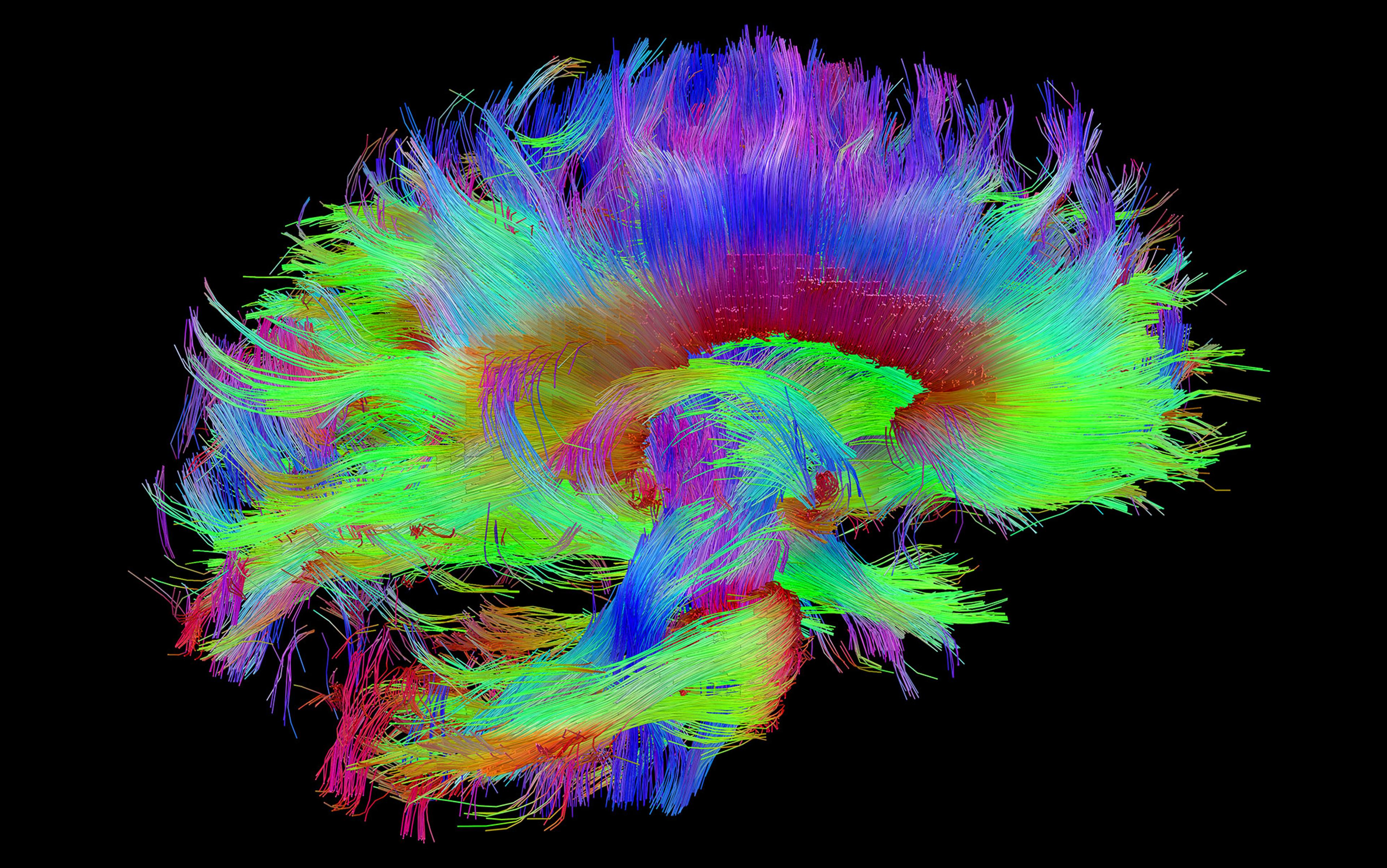
An even more extraordinary perspective comes from patients who are pulled back from death using the new techniques. Some of the most striking research is from Sam Parnia, the director of critical care and resuscitation research at NYU Langone School of Medicine in New York City. Parnia has been looking at resuscitation through hypothermia not only to save his patients, but also to ask some profound questions: when is death final and irreversible? What do we perceive from the other side of death? And when does consciousness really stop? His latest work suggests that consciousness continues for many minutes after the heart stops – and can be extended further by cooling down the brain, slowing cell death and giving doctors a chance to reverse the process and pull the patient back online. Parnia’s studies, many of them enhanced through the use of hypothermia, show that the dying brain is ‘calm and at peace’; as with so many near-death reports collected over the years, the patients in his study describe a welcoming bright light.
Advancements in hypothermia are unsettling, and perhaps that’s why they’ve been such a bone of contention. Part of the resistance is pragmatic: with therapeutic hypothermia comes risk of a huge reduction in blood clotting along with tissue damage from a lack of oxygen; these have contributed to one thing in many accidental hypothermia victims – death. Indeed, these symptoms are known as the ‘triad of death’. Thus, there has been little agreement on how to thread the needle, Varon contends. ‘The temperature time and duration will continue to be debated. Every person is different, so trying to find something that is going to work for everyone is not going to happen,’ he said.
Since the inception of his EPR trial, Tisherman has fought staunch medical criticism. Of particular concern to his colleagues is the blood’s inability to clot under such extreme-cold conditions, an issue that could not be more critical for trauma victims who are pulseless or dying from blood loss. Yet Tisherman responds that his patients are already at high risk of dying. ‘They have an estimated 5 per cent chance of living,’ he says, ‘so why not try something new?’
Another criticism goes to the neurological outcome. What if a patient survives a gunshot or stabbing because of EPR, but suffers permanent, severe brain damage because of an extended period with no oxygen to the brain? ‘That’s an issue with any kind of cardiac arrest, whether there’s trauma or non-trauma,’ Tisherman said. ‘If you have cardiac arrest, whether or not you are in this EPR trial, there’s a chance that you’ll live but that there will be significant brain damage, and that’s a risk of injury regardless of cooling. If what we do increases or decreases that risk, we don’t really know.’ He went on to frame the issue as more a matter of survival. ‘Often resuscitation patients wake up and they live and they’re OK, or they just don’t live. So, we don’t know. Yes, that’s a risk. They’re dying so we need to work on them surviving and waking up.’
The work continues apace. Advancements in hypothermia have put our definition of humanity into question by pushing the boundaries of consciousness and death, and could usher our arrival on other worlds. The therapeutic benefits of hypothermia continue to be discovered and developed along a winding road that enters difficult terrain, but emerges with new traction. Moricheau-Beaupré would be in awe.